By Ed Yong
The Atlantic, July 21, 2022
Jacob Bor has been thinking about a parallel universe. He envisions a world in which America has health on par with that of other wealthy nations, and is not an embarrassing outlier that, despite spending more on health care than any other country, has shorter life spans, higher rates of chronic disease and maternal mortality, and fewer doctors per capita than its peers. Bor, an epidemiologist at Boston University School of Public Health, imagines the people who are still alive in that other world but who died in ours. He calls such people “missing Americans.” And he calculates that in 2021 alone, there were 1.1 million of them.
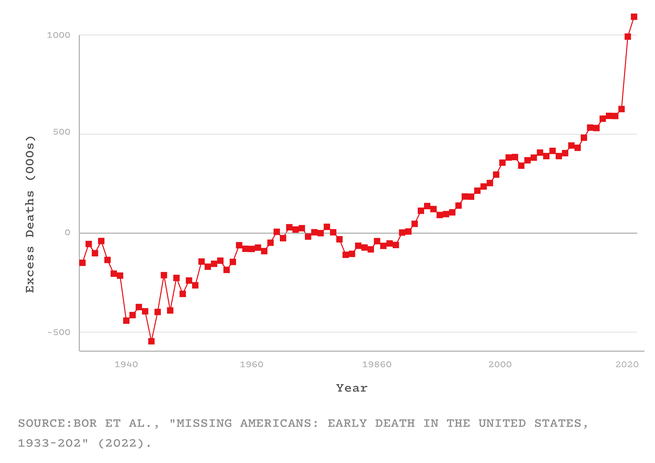
Bor and his colleagues arrived at that number by using data from an international mortality database and the CDC. For every year from 1933 to 2021, they compared America’s mortality rates with the average of Canada, Japan, and 16 Western European nations (adjusting for age and population). They showed that from the 1980s onward, the U.S. started falling behind its peers. By 2019, the number of missing Americans had grown to 626,000. After COVID arrived, that statistic ballooned even further—to 992,000 in 2020, and to 1.1 million in 2021. Were the U.S. “just average compared to other wealthy countries, not even the best performer, fully a third of all deaths last year would have been prevented,” Bor told me. That includes half of all deaths among working-age adults. “Think of two people you might know under 65 who died last year: One of them might still be alive,” he said. “It raises the hairs on the back of my neck.”
These counterfactuals puncture two common myths about America’s pandemic experience: that the U.S. was just one unremarkable victim of a crisis that spared no nation and that COVID disrupted a status quo that was strong and worth restoring wholesale. In fact, as one expert predicted in March 2020, the U.S. had the worst outbreak in the industrialized world—not just because of what the Trump and Biden administrations did, but also because of the country’s rotten rootstock. COVID simply did more of what life in America has excelled at for decades: killing Americans in unusually large numbers, and at unusually young ages. “I don’t think people in the United States actually have any awareness of just how poorly we do as a country at letting people live to old age,” Elizabeth Wrigley-Field, a sociologist at the University of Minnesota, told me.
Although Bor’s study has yet to be formally reviewed, Wrigley-Field and five other independent researchers vouched for its quality to me. “The paper is extremely important, and the researchers who produced this know what they’re doing,” Steven Woolf, a population-health expert at Virginia Commonwealth University, told me. “It builds on, and considerably expands, what we’ve already known.”
Several studies, for example, have shown that America’s life expectancy has tailed behind other comparable countries since the 1970s. By 2010, that gap was already 1.9 years. By the end of 2021, it had grown to 5.3. And although many countries took a longevity hit because of COVID, America was once again exceptional: Among its peers, it experienced the largest life-expectancy decline in 2020 and, unlike its peers, continued declining in 2021. But Bor says that people often misinterpret life-expectancy declines, as if they simply represent a few years shaved off the end of a life. Someone might reasonably ask: What’s the big deal if I die at 76 versus 78? But in fact, life expectancy is falling behind other wealthy nations in large part because a lot of Americans are dying very young—in their 40s and 50s, rather than their 70s and 80s. The country is experiencing what Bor and his colleagues call “a crisis of early death”—a long-simmering tragedy that COVID took to a furious boil.
In every country, the coronavirus wrought greater damage upon the bodies of the elderly than the young. But this well-known trend hides a less obvious one: During the pandemic, half of the U.S.’s excess deaths—the missing Americans—were under 65 years old. Even though working-age Americans were less likely to die of COVID than older Americans, they fared considerably worse than similarly aged people in other countries. From 2019 to 2021, the number of working-age Americans who died increased by 233,000—and nine in 10 of those deaths wouldn’t have happened if the U.S. had mortality rates on par with its peers. “This is a damning finding,” Oni Blackstock, the founder and executive director of Health Justice, told me.
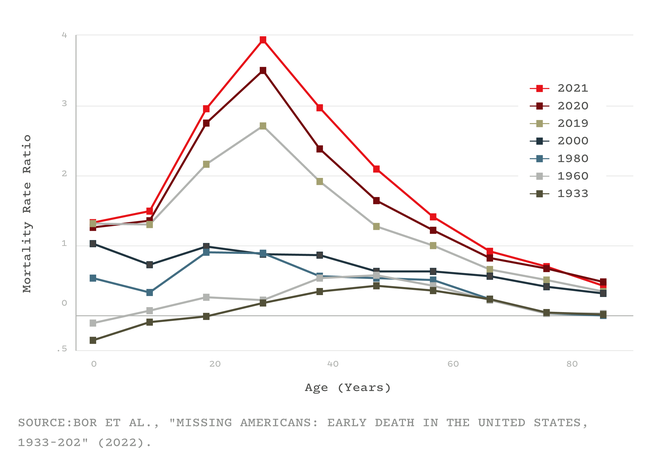
The crisis of early death was evident well before COVID. As many studies and reports have shown, since the turn of the 21st century, “midlife ages are where health and survival in the U.S. really go off the rails,” Wrigley-Field told me. “The U.S. actually does well at keeping people alive once they’re really old,” she said, but it struggles to get its citizens to that point. They might die because of gun violence, car accidents, or heart disease and other metabolic disorders, or drug overdoses, suicides, and other deaths of despair. In all of these, the U.S. does worse than most equivalent countries, both by failing to address these problems directly and by leaving people more vulnerable to them to begin with.
Consider how many years the missing Americans would have collectively enjoyed had they survived—all the birthdays and anniversaries that never happened. In other rich countries, the total “years of life lost” have flatlined for the past five decades. In the U.S., they have soared: In 2021 alone, the 1.1 million missing Americans lost 25 million years of life among them. That number doesn’t account for the events that preceded many of these deaths—the “years of disability, illness, and loss of human potential, creativity, and dignity,” Laudan Aron, a health-policy researcher at the Urban Institute, told me. And, especially in the case of middle-aged deaths, they left behind young dependents, whose own health might suffer as a result. The sheer number of missing Americans, and the “profound ripple effects” of their absence, are “really hard to wrap one’s head around,” Aron said.
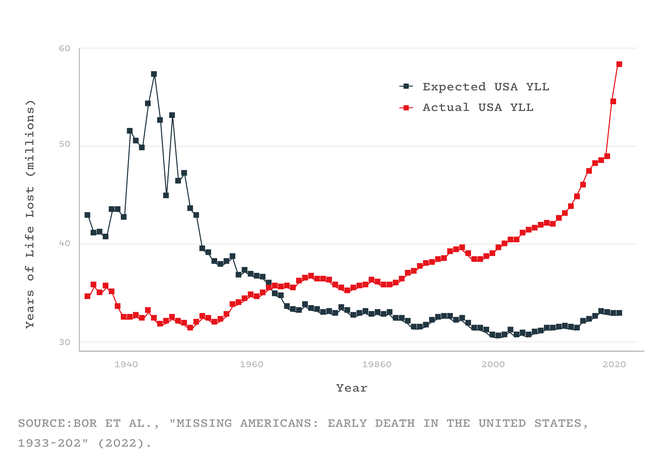
These staggering numbers also help contextualize COVID’s toll. The coronavirus caused the largest single-year rise in mortality since World War II, becoming the third leading cause of death in the U.S., after only heart disease and cancer. But this enormous tragedy unfolded against an already tragic backdrop: The number of missing Americans from 2019 is larger than the number of people who were killed by COVID in 2020 or 2021. This isn’t to minimize COVID’s impact; it simply shows that in the Before Times, America had “very successfully normalized to an extremely high level of death on the scale of what we experienced in the pandemic,” Justin Feldman, a social epidemiologist at Harvard, told me. And when COVID drove those levels skyward, America proved that “we’ll accept even more deaths compared to our already poor historical norms,” Feldman said.
Such deaths, though obvious on a graph, are hidden from Americans with social privilege. In the summer of 2020, Bor remembers having an outdoor BBQ with a friend who grew up in a low-income housing project. “At that point, six months in, he knew six people in his close circle who had been killed by COVID,” Bor told me. “I still don’t.” The fact that half of the working-age Americans who died last year should still be alive “isn’t visceral if you haven’t lost anyone,” he said.
The current mortality crisis was long in the making. In terms of mortality, America’s peer countries—many of which had been hammered by World War II and its aftermath—began catching up with it in the mid-1970s before overtaking in the early 1980s. That was a pivotal era, when globalization, automation, and a growing service industry led to huge losses in mining, manufacturing, and other blue-collar sectors. The U.S. profoundly failed to protect its citizens from these changes. Its social safety net—state assistance for parents, or people facing job, food, or housing insecurity—was meager; its public-health system was languishing after decades of underinvestment; and unlike every other wealthy country, it lacked universal health care. These factors “privatized risk,” Bor and his colleagues wrote in their paper, “tying health more closely to personal wealth and employment.” As labor unions declined and minimum wages stagnated, more Americans had fewer resources to lean on if their health declined. Poorer Americans already lived, on average, shorter lives than rich ones, and that gulf started to widen.
Other particularly American choices exacerbated the stresses on the health of the country’s citizens, again weighing more heavily on less wealthy people. A growing mass-incarceration industry punished them. A deregulatory agenda that began with Ronald Reagan’s administration left them vulnerable to unhealthy foods, workplace hazards, environmental pollutants, guns, and opioids. “America basically says: If you’re poor, you don’t have access to safe choices,” Bor told me.
Factors like social inequalities and frayed social safety nets are the fundamental weaknesses of American society, which more specific problems like opioids, metabolic disorders, and COVID exploit. During the pandemic, for example, poor and minority groups were more likely to be infected because they lived in crowded housing, distrusted medical leaders, and couldn’t work from home or take time off when sick. And instead of addressing these foundational problems, policy makers instead focused on personal responsibility.
America’s drastic underperformance in health also stems from its history of segregation and discrimination. Racist policies have obviously harmed the health of minorities. But as the policy expert Heather McGhee and the physician Jonathan Metzl have independently argued, elites have long marshaled the racial resentment of poor white Americans to undermine support for public goods that would benefit everyone, such as universal health care. Per Frederick Douglass and other Black leaders, “They divided both to conquer each.”
COVID, for example, disproportionately killed Black, Latino, and Indigenous Americans—a trend that, when highlighted to white people, reduces their concern about the pandemic and their support for safety measures. But in 2021, young white Americans still died at three times the rate of the average resident of other peer nations, while young Black and Indigenous Americans died at rates five- and eightfold higher, respectively. “There are thousands of racial-disparity studies that compare Black people to white people—but white Americans are a terrible counterfactual,” Bor told me. They’re frogs in the same pot, boiling more slowly but boiling nonetheless. By using them as a baseline, we ignore how “everyone is harmed by the status quo in the U.S.,” Blackstock told me, while also underestimating how dire things really are for people of color. (The same problem applies to income inequality: White Americans living in the richest 1 percent of counties still have higher rates of maternal and infant mortality than the average residents of wealthy countries.)
So, “what happens now?” Bor asked me. “Are we going to have 1 million missing Americans a year, every year, going forward? Or more?” His study doesn’t suggest a reason for optimism, but it does provide a defense against nihilism. The entire concept of missing Americans is rooted in a comparison with other countries, which shows that these early deaths aren’t inevitable. The U.S. could at least start moving in the direction of its peers by adopting policies that work elsewhere, such as universal health care, minimum-wage increases, federally required paid sick leave, and better unemployment insurance.
But “the inability of our politics to generate policies that manage health threats is grim,” Bor said. None of the weaknesses that COVID exposed have been addressed; some, like the chasm-sized health gaps between rich and poor or white and Black, have been widened. Vaccines significantly reduce the risk of dying from COVID, but their power is blunted by low uptake, new variants, the lifting of almost all infection-thwarting protections, and the looming loss of COVID funding. Reactionary laws that hamstring what public-health departments can do in emergencies will make the U.S. vulnerable to the new viruses that will inevitably assault it in future years. America’s already underperforming health-care system has been badly battered by the pandemic, and weakened by waves of health-care-worker resignations. In recent months, the Supreme Court has constrained both gun and carbon-emission regulations, while clearing the road for states to restrict or ban abortions—a move that could easily boost America’s already sky-high maternal mortality rates. The climate is still changing rapidly, exposing people who have no choice but to work outside to the ravages of heat.
As much of the country returns to normal, Bor’s study makes plain what normal actually meant—and, as I wrote in 2020, that normal led to this. “A lot of Americans may be under the impression that we had a bad go of it during COVID, and once the pandemic is over, they can go back to having the best health in the world,” Woolf told me. “That is a gross misconception.”