Young Adult Insurance Coverage And Out-Of-Pocket Spending: Long-Term Patterns
By Marc L. Berk and Zhengyi Fang
Health Affairs, April 2016From the Abstract
The Affordable Care Act appears to have improved health insurance coverage for young adults (ages 18–30). But data from twenty national surveys conducted between 1977 and 2013 paint a more complex picture, showing coverage rates lower in 2013 than they were thirty-six years earlier.
http://content.healthaffairs.org/content/35/4/734.abstractAlthough the provision in the Affordable Care Act (ACA) that allowed individuals up to age 26 to be covered through their parents’ insurance was partially effective, the rate of coverage for young adults was lower in 2013 than it had been 36 years earlier. Some progress!
The point is the ACA is a series of patches superimposed on our highly fragmented, dysfunctional health care financing system. This patch – extending family coverage into early adult years – fell far short of the one goal of insuring all young adults. In fact, all ACA patches combined are falling far short of our goals of universality, affordability and equity, and we are still left with a highly fragmented, dysfunctional health care financing system.
A improved Medicare that covered everyone would fix this.
Fixing consumer-directed health care by making physicians financial counselors
Study Of Physician And Patient Communication Identifies Missed Opportunities To Help Reduce Patients’ Out-Of-Pocket Spending
By Peter A. Ubel, Cecilia J. Zhang, Ashley Hesson, J. Kelly Davis, Christine Kirby, Jamison Barnett and Wynn G. Hunter
Health Affairs, April 2016
Abstract
Some experts contend that requiring patients to pay out of pocket for a portion of their care will bring consumer discipline to health care markets. But are physicians prepared to help patients factor out-of-pocket expenses into medical decisions? In this qualitative study of audiorecorded clinical encounters, we identified physician behaviors that stand in the way of helping patients navigate out-of-pocket spending. Some behaviors reflected a failure to fully engage with patients’ financial concerns, from never acknowledging such concerns to dismissing them too quickly. Other behaviors reflected a failure to resolve uncertainty about out-of-pocket expenses or reliance on temporary solutions without making long-term plans to reduce spending. Many of these failures resulted from systemic barriers to health care spending conversations, such as a lack of price transparency. For consumer health care markets to work as intended, physicians need to be prepared to help patients navigate out-of-pocket expenses when financial concerns arise during clinical encounters.
From the Introduction
In recent years an increasing number of Americans have chosen health insurance plans with high out-of-pocket expenses, in the form of deductibles, copayments, or coinsurance rates. According to economic theory, such plans should make consumers more sensitive to the price of health care services. Indeed, copayments have been shown to reduce health care use. However, high out-of-pocket spending can also create financial burdens for patients. In 2014 one in three Americans reported having difficulty paying health care bills. Many patients did not adhere to prescribed health care interventions because of difficulty paying for them. In addition, some patients reported that the financial burden of paying for medical care caused them to miss mortgage payments or led them to personal bankruptcy.
On the one hand, patients with high out-of-pocket spending have an opportunity to behave as informed consumers in the health care Marketplace. On the other hand, their status as consumers exposes them to potential financial burden. Ideally, patients will recognize this trade-off between the medical benefits and the financial costs of receiving health care services, incurring out-of-pocket expenses only when the benefits of receiving the services outweigh the costs.
In this article we present a qualitative content analysis of health care spending discussions from outpatient clinic visits for patients with breast cancer, rheumatoid arthritis, or depression who saw specialists who treat these conditions. We present a series of physician behaviors that interfered with patients’ efforts to either lower their out-of-pocket expenses or understand the pros and cons of less costly health care alternatives.
From the Study Results
Our qualitative content analysis revealed two broad categories of physician behaviors that led to missed opportunities to reduce out-of-pocket expenses. The first set of behaviors involved the physician’s failure to address the patient’s financial concerns, in which the physician did not make an explicit effort to either acknowledge or deal with the seriousness of the patient’s concerns. The second category involved instances where physicians did make explicit efforts to deal with patients’ financial concerns but failed to resolve such concerns satisfactorily.
From the Discussion
Many health care policies are ultimately played out “at the bedside,” by influencing the way doctors and patients make medical decisions. In the case of policies promoting health care consumerism, many patients are faced with important decisions about whether the benefits of health care interventions justify their financial cost. In this qualitative, observational study of outpatient interactions, we identified a range of physician behaviors that stand in the way of helping patients make informed decisions about ways to potentially lower their out-of-pocket spending. Some behaviors reflect physicians’ failures to fully engage with patients’ financial concerns, from never acknowledging such concerns, to dismissing them too quickly, to getting sidetracked discussing frustration with a system that creates such high out-of-pocket spending. Other behaviors reflect physicians’ efforts to engage patients about their financial concerns but efforts that potentially fall short, because physicians fail to resolve uncertainty about out-of-pocket expenses or turn to temporary solutions without making long-term plans to reduce patients’ spending.
We recognize that physician-patient communication is a two-way street and that some of the failures described here resulted in part from patients having difficulty clearly and explicitly expressing their financial concerns. Patients have difficulty partly because health care consumerism is a relatively recent phenomenon in the United States for most people, meaning that patients have not had substantial experience that would help them become savvier about the health care marketplace. Nevertheless, it is still incumbent on physicians to do their best to overcome patients’ difficulties communicating about their expenses.
We acknowledge that many of the potential failures we have identified here, if they truly do reflect physician failure, also reflect more general failure of the US health care system. Physicians in the United States have difficulty factoring financial concerns into health care decisions in part because out-of-pocket spending is often difficult to determine and health care prices are often opaque. Consequently, physicians under time constraints cannot be expected to fully resolve patients’ financial concerns in the space of any single outpatient appointment.
From the Conclusion
Ideally, when people face high out-of-pocket spending for health care services, they will act like savvy consumers, exploring the pros and cons of their alternatives with full knowledge of the financial consequences of those alternatives. This confidence is undermined whenever clinical interactions lead patients to miss opportunities to explore less costly alternatives or to identify means by which they can receive their current interventions at lower prices.
http://content.healthaffairs.org/content/35/4/654.abstract
***
Comment:
By Don McCanne, M.D.
Although the theme of this article seems to be that physicians should improve their skills in communicating with patients about their out-of-pocket spending for health care in order to enable spending reductions that are the goal of the ever-increasingly prevalent consumer-directed health care plans. But there is a much more important message buried in this study. Physicians do not have the time nor the tools and are basically incapable of assisting patients with their burdensome cost sharing.
Patients are mostly on their own to try to negotiate past the financial barriers to care, or, failing to do so, accept the fact that they may have to forgo the recommended health care simply because they cannot afford to pay for it. Training physicians in personal financial management so that they can counsel patients on how they can manage their deductibles and other expenses, and then expecting physicians to dedicate a significant portion of the patient interaction time to that counseling are just not practical uses of the very limited time the physician has with the patient – time that should be fully dedicated to managing the patient’s medical problems.
Also buried in the full article is this comment: “From this sample of 3,000 transcripts, we excluded visits that were conducted by primary care physicians, nurse practitioners, or nurses because these clinicians are often not the ones that prescribed the expensive interventions relevant to the diseases in question.”
Wow! Primary care was excluded because that is not where the expensive interventions occur? So primary care really does provide greater value? Yet most primary care (except sometimes certain preventive services) falls below today’s higher deductibles, and thus the patient is quite sensitive to primary care costs because it usually lacks first dollar coverage.
It is not the lack of training of health care professionals in patient-consumer financial counseling that is the problem. It is the transfer of financial responsibility to the patient that is causing the difficulties. Many other nations that spend much less on health care than we do are able to provide first dollar coverage. We can as well. We can control costs in a much more patient-friendly manner through an improved Medicare that covers everyone.
Fixing consumer-directed health care by making physicians financial counselors
Study Of Physician And Patient Communication Identifies Missed Opportunities To Help Reduce Patients’ Out-Of-Pocket Spending
By Peter A. Ubel, Cecilia J. Zhang, Ashley Hesson, J. Kelly Davis, Christine Kirby, Jamison Barnett and Wynn G. Hunter
Health Affairs, April 2016Abstract
Some experts contend that requiring patients to pay out of pocket for a portion of their care will bring consumer discipline to health care markets. But are physicians prepared to help patients factor out-of-pocket expenses into medical decisions? In this qualitative study of audiorecorded clinical encounters, we identified physician behaviors that stand in the way of helping patients navigate out-of-pocket spending. Some behaviors reflected a failure to fully engage with patients’ financial concerns, from never acknowledging such concerns to dismissing them too quickly. Other behaviors reflected a failure to resolve uncertainty about out-of-pocket expenses or reliance on temporary solutions without making long-term plans to reduce spending. Many of these failures resulted from systemic barriers to health care spending conversations, such as a lack of price transparency. For consumer health care markets to work as intended, physicians need to be prepared to help patients navigate out-of-pocket expenses when financial concerns arise during clinical encounters.
From the Introduction
In recent years an increasing number of Americans have chosen health insurance plans with high out-of-pocket expenses, in the form of deductibles, copayments, or coinsurance rates. According to economic theory, such plans should make consumers more sensitive to the price of health care services. Indeed, copayments have been shown to reduce health care use. However, high out-of-pocket spending can also create financial burdens for patients. In 2014 one in three Americans reported having difficulty paying health care bills. Many patients did not adhere to prescribed health care interventions because of difficulty paying for them. In addition, some patients reported that the financial burden of paying for medical care caused them to miss mortgage payments or led them to personal bankruptcy.
On the one hand, patients with high out-of-pocket spending have an opportunity to behave as informed consumers in the health care Marketplace. On the other hand, their status as consumers exposes them to potential financial burden. Ideally, patients will recognize this trade-off between the medical benefits and the financial costs of receiving health care services, incurring out-of-pocket expenses only when the benefits of receiving the services outweigh the costs.
In this article we present a qualitative content analysis of health care spending discussions from outpatient clinic visits for patients with breast cancer, rheumatoid arthritis, or depression who saw specialists who treat these conditions. We present a series of physician behaviors that interfered with patients’ efforts to either lower their out-of-pocket expenses or understand the pros and cons of less costly health care alternatives.
From the Study Results
Our qualitative content analysis revealed two broad categories of physician behaviors that led to missed opportunities to reduce out-of-pocket expenses. The first set of behaviors involved the physician’s failure to address the patient’s financial concerns, in which the physician did not make an explicit effort to either acknowledge or deal with the seriousness of the patient’s concerns. The second category involved instances where physicians did make explicit efforts to deal with patients’ financial concerns but failed to resolve such concerns satisfactorily.
From the DiscussionMany health care policies are ultimately played out “at the bedside,” by influencing the way doctors and patients make medical decisions. In the case of policies promoting health care consumerism, many patients are faced with important decisions about whether the benefits of health care interventions justify their financial cost. In this qualitative, observational study of outpatient interactions, we identified a range of physician behaviors that stand in the way of helping patients make informed decisions about ways to potentially lower their out-of-pocket spending. Some behaviors reflect physicians’ failures to fully engage with patients’ financial concerns, from never acknowledging such concerns, to dismissing them too quickly, to getting sidetracked discussing frustration with a system that creates such high out-of-pocket spending. Other behaviors reflect physicians’ efforts to engage patients about their financial concerns but efforts that potentially fall short, because physicians fail to resolve uncertainty about out-of-pocket expenses or turn to temporary solutions without making long-term plans to reduce patients’ spending.
We recognize that physician-patient communication is a two-way street and that some of the failures described here resulted in part from patients having difficulty clearly and explicitly expressing their financial concerns. Patients have difficulty partly because health care consumerism is a relatively recent phenomenon in the United States for most people, meaning that patients have not had substantial experience that would help them become savvier about the health care marketplace. Nevertheless, it is still incumbent on physicians to do their best to overcome patients’ difficulties communicating about their expenses.
We acknowledge that many of the potential failures we have identified here, if they truly do reflect physician failure, also reflect more general failure of the US health care system. Physicians in the United States have difficulty factoring financial concerns into health care decisions in part because out-of-pocket spending is often difficult to determine and health care prices are often opaque. Consequently, physicians under time constraints cannot be expected to fully resolve patients’ financial concerns in the space of any single outpatient appointment.
From the Conclusion
Ideally, when people face high out-of-pocket spending for health care services, they will act like savvy consumers, exploring the pros and cons of their alternatives with full knowledge of the financial consequences of those alternatives. This confidence is undermined whenever clinical interactions lead patients to miss opportunities to explore less costly alternatives or to identify means by which they can receive their current interventions at lower prices.
Although the theme of this article seems to be that physicians should improve their skills in communicating with patients about their out-of-pocket spending for health care in order to enable spending reductions that are the goal of the ever-increasingly prevalent consumer-directed health care plans. But there is a much more important message buried in this study. Physicians do not have the time nor the tools and are basically incapable of assisting patients with their burdensome cost sharing.
Patients are mostly on their own to try to negotiate past the financial barriers to care, or, failing to do so, accept the fact that they may have to forgo the recommended health care simply because they cannot afford to pay for it. Training physicians in personal financial management so that they can counsel patients on how they can manage their deductibles and other expenses, and then expecting physicians to dedicate a significant portion of the patient interaction time to that counseling are just not practical uses of the very limited time the physician has with the patient – time that should be fully dedicated to managing the patient’s medical problems.
Also buried in the full article is this comment: “From this sample of 3,000 transcripts, we excluded visits that were conducted by primary care physicians, nurse practitioners, or nurses because these clinicians are often not the ones that prescribed the expensive interventions relevant to the diseases in question.”
Wow! Primary care was excluded because that is not where the expensive interventions occur? So primary care really does provide greater value? Yet most primary care (except sometimes certain preventive services) falls below today’s higher deductibles, and thus the patient is quite sensitive to primary care costs because it usually lacks first dollar coverage.
It is not the lack of training of health care professionals in patient-consumer financial counseling that is the problem. It is the transfer of financial responsibility to the patient that is causing the difficulties. Many other nations that spend much less on health care than we do are able to provide first dollar coverage. We can as well. We can control costs in a much more patient-friendly manner through an improved Medicare that covers everyone.
Why Do We Pay So Much for Health Care – But Get Such Poor Results?
By N.F. Hanna, M.D.
New York Observer, April 5, 2016
As a primary care physician practicing for three decades in the same location, I have had the privilege of seeing patients regularly across a span of many years. I have celebrated my patients’ joys and triumphs, but also mourned with them in their deepest tragedies and sorrows. I have shared and continue to share in their trials and vulnerabilities, and often as more than their doctor; patients sometimes confide in me things they do not even share with their families.
The result: I have encountered far too many heartbreaking stories, more than enough to be certain that our health care system is deeply broken. Too many patients watching their savings disappear overnight in the face of staggering medical bills, even those resulting from low-quality care. Too many people working tirelessly for the false promise that health insurance equals financial security. Too many families living in fear of slipping into poverty because of one illness. The physical, financial, and emotional pain is often unbearable, creating a bitterly vicious cycle that continues to spiral downward.
These stories are sobering reminders that as nationwide debates about health care in America amplify again during this election season, real-life casualties of our broken system suffer quietly. The mainstream conversation is often frustratingly complex and politically-driven. Meanwhile, in the midst of a fray of political demagoguery and confusion, countless American families are struggling at the hands of a system they may not fully understand.
The heart of the problem with the American health care system can be boiled down to one troubling question: why are Americans paying much more per person for health care than those in other developed nations, but getting much less in terms of quality? As a physician with over 40 years of experience practicing medicine in the United States and the United Kingdom, I naturally view this tragic “pay more, get less” paradox through a clinician’s eyes. As is taught in medical school, it all starts with carefully diagnosing the problem.
Let us start with diagnosing the “pay more” element of the paradox. First, the facts: we are paying far more for health care than any other Western industrial nation. Consider that in 2012 the U.S. paid $8,745 per person on health care. This was double what was paid on health care per person in most developed countries in the world, including France and the U.K. Spending growth has continued, and the U.S. today spends about $10,000 per person annually. As a direct consequence, many sources site medical bills as the number one cause of personal bankruptcies (which are akin to financial “death”) across the U.S. A study in The American Journal of Medicine found that 62 percent of all 2007 bankruptcies, using a conservative definition, were medical bankruptcies. Sadly insurance is not enough to offer protection; over three-quarters (78 percent) of medical debtors were insured at the onset of their illness. And this is a crisis not only on the personal and family level, but also on the national level. Health care spending in the U.S. has increased dramatically over the years and continues to grow.
What is behind these staggering costs? I explore several primary factors that are discussed in depth in my book, “Dying of Health Care.” The first four of these factors are caused by doctors and the latter five are caused by other players in the system, leaving doctors and patients alike as victims: excessive testing, overprescribing, direct-to-specialist referrals and consultations, doctors not assessing costs to the system overall, health insurance and medical billing industry waste, overpriced pharmaceuticals and medical devices, direct-to-consumer pharmaceutical advertising, increasing administrative costs for medical practices, and a fragmented hospital system.
One of these factors that is a particularly tough pill to swallow is the cost of health insurance and medical billing. Health insurance companies are like a middleman between providers and patients, so their costs should be kept as low as possible since the money is not being used to care for patients directly. Unfortunately, the costs are astronomical and far greater than in other nations. Because of how difficult insurance companies have made it for providers to get paid for their services (their incentive is to maximize their profits), they have in effect created their own menace: medical billing companies. Fifteen years ago, I had never heard of the medical billing business, but today it is one of the most thriving components in the health care industry. If insurance companies are like the middleman between providers and patients, medical billing companies are like the middleman to the middleman; both of them take a significant cut of your health care dollars. As a poignant example of the heavy burden that medical billing codes and processes create, Duke University Hospital at one point had 900 beds for patients … compared to its 1,300 billing clerks.
Another important factor to highlight briefly is excessive testing, which has multiple causes. Unfortunately, testing begets more testing, as one test often leads to a desire to order other follow-up testing due to coincidental findings. And these tests sometimes lead to unnecessary invasive procedures, which can harm or even kill a patient. Excessive testing, of course, also costs a great deal of money at the same time, thus contributing to both sides of the “pay more, get less” paradox.
Now, on to the “get less” half of the paradox. It would seem reasonable that the U.S. spends far more on health care than any other nation in the world, so long as our health results are the best in the world as well. Unfortunately, this is very far from the truth. That American patients are “getting less” in terms of quality is not a question to debate. To evaluate this, there are several studies that consider a variety of health metrics and rank the health care systems of nations around the world. The common conclusion across all of them: the U.S. is not delivering the quality that the price tag would suggest. And, truthfully, it is not even close. As just one example, a 2014 study ranked the health care systems of 11 developed nations, considering factors such as quality of care and access to doctors. It found that the U.S. ranked last overall. Within particular subcategories, studies have shown that the U.S. ranks 25th out of the 34 developed countries in the Organization for Economic Cooperation and Development (OECD) in terms of hospital beds per 1,000 people, and it ranks 28th in doctors per 1,000 people.
In my opinion, life expectancy is the best metric to consider in evaluating a health care system because it is the cumulative effect of all aspects of health. Sadly, our life expectancy ranks 27th among the 34 OECD nations. So, let us bring together our analysis of the “pay more” and “get less” components. The U.S. spent $8,745 per person in total health expenditures in 2012, as discussed, and its total population life expectancy at birth was 78.7 years. Compare this to Spain, which spent $2,998 per person and achieved a life expectancy of 82.5 years. Take a look at the chart below, which plots the life expectancy of several countries against per-person health care spending. In reading the chart, the most efficient and effective systems fall in the upper left area. From our conversation thus far, you would expect the U.S. to be an outlier in that its system is so expensive and not as effective. But saying it is an outlier is a major understatement.
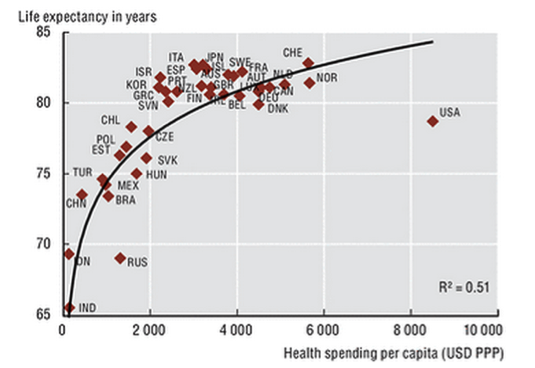
Life expectancy at birth and health spending per capita (Source: OECD Health Statistics, World Bank for non-OECD countries)
Note particularly how far the U.S.’s life expectancy mark falls below the trend curve, which is where you would expect it to fall based on its amount of spending. Clearly, something is seriously amiss.
Perhaps the saddest element of “getting less”: iatrogenic diseases, or diseases caused by medical or surgical intervention, are a major issue in the U.S. In her commentary in The Journal of the American Medical Association, Dr. Barbara Starfield of Johns Hopkins University, citing three previous studies, estimated the number of American deaths due to iatrogenic causes to be 225,000 per year. In other words, about 225,000 American deaths per year are actually caused by medical care. If classified as such, this would make iatrogenic causes the third most common cause of death in the United States, after heart disease and cancer. To make matters worse, as Dr. Starfield points out, these numbers may actually be on the lower end of comparable estimations, and they only include iatrogenic diseases that directly lead to death. Indeed, iatrogenic diseases are a contributor to our disappointingly low life expectancy numbers as well as the high cost of our health care.
The consequences of our painful paradox – the heartbreaking stories I mentioned at the beginning – are real and they are tragic. Over the years, I have seen that the physical, emotional, and financial health of a patient are closely tied together. All three aspects are crucially and inseparably intertwined; any one of the three can adversely, or positively, affect the other two. Too many times I have seen serious, unexpected illnesses – in addition to physically threatening my patients’ health – eliminating their financial security. Of course, when these patients find themselves without the means to support their families or sometimes to even survive, there is an unbearable psychological impact and that, in turn, affects their physical health.
The urgency to act has never been greater. We have traveled through 100 years of band-aid health care reform attempts, leading up to a confusing mix of mostly private and some public care. The most recent and perhaps the most controversial reform, the Affordable Care Act, is not a viable solution to mend our system. We are still on a path of financial un-sustainability, and people’s premiums, co-payments, co-insurances, and deductibles have only risen. As author of the best-selling “America’s Bitter Pill,” Steven Brill, explained, “Put simply, with Obamacare we’ve changed the rules related to who pays for what, but we haven’t done much to change the prices we pay.”
The reality is that there are solutions that can work to heal our ailing system that both improve the quality and reduce the cost of our health care. These include implementing a more standardized system of medical decision-making that takes into account cost and empirically proven effectiveness, which would smooth out the wide divergences that come from the subjectivity of medical decision-making. A single-payer system for all, in my view, is a critical solution that will rein in our costs and improve our care by eliminating the waste surrounding insurance and medical billing companies, creating negotiating power for cheaper pharmaceuticals and medical devices (these are far more expensive in the U.S. than abroad), uniting electronic health records to reduce inefficiencies, changing the way doctors are paid away from the fee-for-service system (which rewards for quantity of care, regardless of effectiveness), and overseeing the standardization discussed previously. The truth, in fact, is that the United States is almost totally alone among developed nations in lacking universal health care.
Regardless of your perspective on the appropriate treatment for our health care woes, we as a nation must be knowledgeable and engaged about the subject. We must be aware of the distressful, painful stories of Americans (including, I am sure, many of the people reading this article) who have been victims of a broken system. We must boldly look through the cloud of political posturing and journalistic sensationalism and stand up for the health of our children, our parents, our brothers, and our sisters.
The diagnosis is daunting, but clear. We must together rise above politics and treat this cancer inside us.
N.F. Hanna, M.D. is a primary care physician with nearly 40 years of experience practicing medicine in the U.S. and U.K. He is the author of the newly released book, Dying of Health Care: How the System Harms Americans Physically and Financially, and How to Change It.
http://observer.com/2016/04/why-do-we-pay-so-much-for-healthcare-but-get-such-poor-results/
The Salt Lake Tribune editors make case for Medicare for all
High costs of hepatitis medicine make a good case for universal Medicare
Editorial
The Salt Lake Tribune, April 4, 2016
Those who continue to argue that there is a “free market solution” to the unconscionable costs and gaps in the American health care system have to explain away the train wreck surrounding new cures for hepatitis C.
The good news is that there is a cure for hepatitis C, a blood disease that can lead to a slow and painful death as it destroys a victim’s liver. In fact, now there are a few. Gilead Sciences markets concoctions called Sovaldi and Harvoni. Janssen Research offers a drug called Olysio.
The bad news is that the cost of the full treatment regimen for a single patient can run from $83,000 to $189,000. That, obviously, is well beyond the reach of nearly every household and understandably enough to scare off both private insurance carriers and government-funded Medicaid.
The worse news is that, because the United States clings to the idea that wellness is a commodity subject to rational market forces, nobody is trying to limit these awful costs.
The drug companies charge so much for these medications for one reason: Because they can.
Functioning free markets do not — and never will — exist in health care because the sellers so often hold all the cards.
Civilized nations — a term that excludes the United States when discussing health care — either regulate the prices of drugs or use their concentrated purchasing power to negotiate a reasonable cost.
Drug makers argue that even the staggering cost of Sovaldi or related drugs is a bargain compared to avoided costs of more treatment, surgeries, disability, early death, etc.
It is notable that single-payer systems, such as in the United Kingdom, have done the math and agreed to pay high — though less than in the U.S. — prices for these drugs. That’s because, in those nations, the single payer does, indeed, come out ahead by paying a lot now but saving many multiples of that later.
In other words, the case made by the drug companies for allowing them to charge such high prices is also an argument for Medicare for all.
http://www.sltrib.com/opinion/3738478-155/editorial-high-costs-of-hepatitis-medicine
***
Comment:
By Don McCanne, M.D.
If there is any good in the fact that drug companies are gouging patients and payers it is that the citizenry may finally awaken to the fact that we need the government involved to straighten out this crisis, and, by extension, that we can finally get past the anti-government hangup preventing us from enacting a single payer system. We can thank the editors of The Salt Lake Tribune for reminding us that the solution we need is a single payer Medicare for all.
The Salt Lake Tribune editors make case for Medicare for all
High costs of hepatitis medicine make a good case for universal Medicare
Editorial
The Salt Lake Tribune, April 4, 2016Those who continue to argue that there is a “free market solution” to the unconscionable costs and gaps in the American health care system have to explain away the train wreck surrounding new cures for hepatitis C.
The good news is that there is a cure for hepatitis C, a blood disease that can lead to a slow and painful death as it destroys a victim’s liver. In fact, now there are a few. Gilead Sciences markets concoctions called Sovaldi and Harvoni. Janssen Research offers a drug called Olysio.
The bad news is that the cost of the full treatment regimen for a single patient can run from $83,000 to $189,000. That, obviously, is well beyond the reach of nearly every household and understandably enough to scare off both private insurance carriers and government-funded Medicaid.
The worse news is that, because the United States clings to the idea that wellness is a commodity subject to rational market forces, nobody is trying to limit these awful costs.
The drug companies charge so much for these medications for one reason: Because they can.
Functioning free markets do not — and never will — exist in health care because the sellers so often hold all the cards.
Civilized nations — a term that excludes the United States when discussing health care — either regulate the prices of drugs or use their concentrated purchasing power to negotiate a reasonable cost.
Drug makers argue that even the staggering cost of Sovaldi or related drugs is a bargain compared to avoided costs of more treatment, surgeries, disability, early death, etc.
It is notable that single-payer systems, such as in the United Kingdom, have done the math and agreed to pay high — though less than in the U.S. — prices for these drugs. That’s because, in those nations, the single payer does, indeed, come out ahead by paying a lot now but saving many multiples of that later.
In other words, the case made by the drug companies for allowing them to charge such high prices is also an argument for Medicare for all.
http://www.sltrib.com/opinion/3738478-155/editorial-high-costs-of-hepatitis-medicine
If there is any good in the fact that drug companies are gouging patients and payers it is that the citizenry may finally awaken to the fact that we need the government involved to straighten out this crisis, and, by extension, that we can finally get past the anti-government hangup preventing us from enacting a single payer system. We can thank the editors of The Salt Lake Tribune for reminding us that the solution we need is a single payer Medicare for all.
Anthem and Dignity collude with employers, shafting employees
Anthem Blue Cross, Dignity Health Partner to Improve Health, Lower Employer Costs
Business Wire, March 31, 2016
Anthem Blue Cross and Dignity Health, one of the largest hospital systems in the country, have collaborated to introduce a new tiered EPO/PPO plan designed to improve employee health and lower costs through an integrated care management system.
The Premier Tiered EPO/PPO product is designed for self-insured large groups, or employers with more than 101 employees and will launch on May 1, 2016 in Ventura County.
The plans are designed to offer choice and flexibility for employees who are members. They can select from either the Exclusive Provider Organization (EPO) that provides the best price with a pre-determined network of high value Dignity Health providers, or a Preferred Provider Organization (PPO) which provides access to a wider range of providers to choose from at varying copay and cost share levels. The new product combines the managed care capabilities and expertise of both organizations, with a focus on clinical quality, access and efficiency of health care services.
“As health care providers, we understand the challenges employers face in managing health care access and cost of care,” said Duncan Ross, Dignity Health Vice President, Employer Relations. “This collaboration with Anthem creates a care management model that will help employers reduce costs and provide a better patient experience for their employees, and reflects our mission of service and commitment to our communities.”
***
Comment:
By Don McCanne, M.D.
In announcing their new program that will “improve health and lower employer costs,” Anthem Blue Cross and Dignity Health show us once again that by relying on the private sector to control health care financing, we will continue to see innovations that serve their industries well, but at a cost to patients.
In this case Anthem and Dignity are providing a competitively priced product that will be cheaper for employers, but it will cause employees to choose between either an exclusive provider organization with severe restrictions in choice of providers or a preferred provider organization with moderate restrictions in provider choice but greater exposure to out-of-pocket spending. Either choice is worse for the employees than under more typical employer-sponsored plans of the past.
Under a well-designed single payer system, patients would have choice of their health care professionals and hospitals, and financial barriers would be removed by providing first dollar coverage. Many other features of a single payer system would control costs in a patient-friendly manner.
Anthem and Dignity collude with employers, shafting employees
Anthem Blue Cross, Dignity Health Partner to Improve Health, Lower Employer Costs
Business Wire, March 31, 2016
Anthem Blue Cross and Dignity Health, one of the largest hospital systems in the country, have collaborated to introduce a new tiered EPO/PPO plan designed to improve employee health and lower costs through an integrated care management system.
The Premier Tiered EPO/PPO product is designed for self-insured large groups, or employers with more than 101 employees and will launch on May 1, 2016 in Ventura County.
The plans are designed to offer choice and flexibility for employees who are members. They can select from either the Exclusive Provider Organization (EPO) that provides the best price with a pre-determined network of high value Dignity Health providers, or a Preferred Provider Organization (PPO) which provides access to a wider range of providers to choose from at varying copay and cost share levels. The new product combines the managed care capabilities and expertise of both organizations, with a focus on clinical quality, access and efficiency of health care services.
“As health care providers, we understand the challenges employers face in managing health care access and cost of care,” said Duncan Ross, Dignity Health Vice President, Employer Relations. “This collaboration with Anthem creates a care management model that will help employers reduce costs and provide a better patient experience for their employees, and reflects our mission of service and commitment to our communities.”
In announcing their new program that will “improve health and lower employer costs,” Anthem Blue Cross and Dignity Health show us once again that by relying on the private sector to control health care financing, we will continue to see innovations that serve their industries well, but at a cost to patients.
In this case Anthem and Dignity are providing a competitively priced product that will be cheaper for employers, but it will cause employees to choose between either an exclusive provider organization with severe restrictions in choice of providers or a preferred provider organization with moderate restrictions in provider choice but greater exposure to out-of-pocket spending. Either choice is worse for the employees than under more typical employer-sponsored plans of the past.
Under a well-designed single payer system, patients would have choice of their health care professionals and hospitals, and financial barriers would be removed by providing first dollar coverage. Many other features of a single payer system would control costs in a patient-friendly manner.
Medical Students Call for Single-Payer Health Insurance
By Mark Chee, Rebecca Gieseker and Rachel Stones
Chicago Maroon, March 31, 2016
As medical students, we have chosen a profession dedicated to treating illness and helping people live healthy lives.
Yet, early on during our training, we learn about the unequal access to care, unaffordable treatments, and medical debt that patients face because of our current private, for-profit health insurance system. We hear about physicians who are increasingly burdened with paperwork and frustrated by a system that does not serve their patients. We discover that despite spending more per capita on health care than other developed countries, the U.S. population has a shorter life expectancy, higher infant mortality, and worse overall health.
While the implementation of the Affordable Care Act (ACA) has expanded coverage, it fails to sufficiently address the problems our health care system faces. Around 33 million Americans remain uninsured, some indefinitely. These individuals are immigrants, who still cannot afford health insurance or live in states that have blocked Medicaid expansion. In addition to this remaining lack of coverage, increasing deductibles and cost sharing are also being used to shift the financial burden from insurers to patients. Over 50 percent of bankruptcy filings in the U.S. are due to illness and medical debt, even though the majority of individuals in this group has some form of coverage when they file for bankruptcy. Expanding insurance coverage that leaves patients vulnerable to the financial burden of illness is not the answer. Furthermore, narrow network health plans prevent patients from having continuity of care with their physicians and expose them to exorbitant (and often unexpected) out-of-network costs.
Medical students often ask what can be done about this. The clear solution is a single-payer health care reform. In a single-payer system, Medicare would be expanded to cover all U.S. residents, but care would continue to be delivered by private institutions. This would guarantee access to health care for the 33 million Americans who remain uninsured under the ACA, cover necessary services without co-pays, coinsurance, or deductibles, and contain health care costs by reducing the high administrative costs of for-profit insurers. While a single-payer wouldn’t solve all the problems that our health care system faces, it would be an important first step to make our health system more equitable, affordable, and efficient.
Implementing single-payer, or Improved Medicare for All, is far from revolutionary, and it can work in the U.S. We already spend more money than other countries that have implemented universal coverage. Furthermore, public opinion favors this approach. Recent polls have found that 58 percent of the U.S. population supports the idea of Medicare-for-all. Here at the Pritzker School of Medicine, a fall 2015 survey distributed by the school’s chapter of Physicians for a National Health Program (PNHP) identified 108 medical students and 119 physicians/faculty (including at least seven deans and six third-year clerkship directors) who publically supported single-payer. While many argue that single-payer would be too expensive for patients and the government, an economic analysis of the single-payer bill HR 676 in the U.S. House of Representatives showed that 95 percent of Americans would actually save money.
As a key hospital on the South Side of Chicago, single-payer could benefit rather than harm the bottom line for the University of Chicago Medicine. During the discussions around the Level I trauma center, a main argument brought forth against the expansion of the University’s emergency department involved the need to have a financially viable patient mix. Since Medicare and Medicaid reimbursement often do not cover the full cost of treating a patient, privately insured patients are needed to subsidize this uncompensated care. A trauma center would likely be used by patients in the surrounding communities who are insured by Medicare or Medicaid or are otherwise uninsured. Under a single-payer health care system, varying rates of reimbursements would not be an issue, and there would no longer be a financial incentive to serve the wealthy over the underinsured and vulnerable.
As doctors-in-training, we are excited to devote our futures to serving others, but we have already seen the struggles and burnout faced by providers and patients under our fragmented, expensive, and inefficient system. We want to practice medicine in a system that serves all Americans and guarantees health care as a basic human right for all. Those who stand to lose from single-payer in the U.S. have significant voices in the political sphere and include the for-profit insurance companies and their stakeholders, Big Pharma, and political leaders who benefit from the current status quo. However, as the next generation of physicians, if we stand together and make our voices heard, single-payer will be achieved in our lifetime.
Mark Chee, Rebecca Gieseker, and Rachel Stones are medical students at the Pritzker School of Medicine at the University of Chicago.
http://chicagomaroon.com/2016/03/31/paying-less-with-single-payer/
Oklahoma physician leaders vote to abandon Medicaid patients
Oklahoma State Medical Association urges doctors to mull leaving Medicaid over 25 percent rate cut
By Barbara Hoberock
Tulsa World, April 1, 2016
Oklahoma State Medical Association leaders have voted unanimously to urge members to consider dropping out of Medicaid.
The association’s executive committee took the unanimous vote on Wednesday following an announcement earlier in the week by the Oklahoma Health Care Authority that Medicaid rates could be cut by as much as 25 percent effective June 1.
For the current fiscal year, the state has seen a deepening revenue failure requiring state-appropriated agencies to make cuts.
“We are fully aware this will create an access-to-care crisis for rural residents, vulnerable seniors, the disabled and the nearly 60 percent of Oklahoma babies born under Medicaid,” said OSMA President Woody Jenkins. “But a 25 percent rate cut, combined with previous cuts that had already been made in recent years, will leave many of our members with little choice.”
He said the association in coming days will be offering guidance on its website for doctors on how to opt out of the Medicaid program.
***
KGOU Update:
The third part of the plan would restore the Medicaid reimbursement rate to 86.5 percent of Medicare. Earlier this week, the Oklahoma Health Care Authority proposed reducing the reimbursement rate to providers by 25 percent as a result of the estimated $1.3 billion general revenue shortfall in the upcoming fiscal year.
http://kgou.org/post/oklahoma-health-care-authority-proposes-plan-insure-more-oklahomans#stream/0
***
Comment:
By Don McCanne, M.D.
One of the flaws in our fragmented, multi-payer system of financing health care is that low-income patients tend to be lumped into the Medicaid program. Since it is a welfare program serving individuals who do not command much political capital, politicians are more willing to use cuts in Medicaid to balance their budgets than cuts for programs designed to serve the general population such as Medicare and Social Security. What lessons can Oklahoma’s proposed 25 percent cut in Medicaid rates provide for us?
As a welfare program, Medicaid does remain chronically underfunded. As such, access problems occur because of a lack of willing providers since there is reluctance on the part of others to accept the lower Medicaid rates. But should the less fortunate members of society be relegated to a lower standard of health care, or should everyone have the equivalent access to essential health care services? That question has been answered by our politicians even if it was never asked.
That said, what response should organized medicine have to these cuts in Medicaid? Perhaps we should ask whom they perceive as being victimized here. The Oklahoma State Medical Association (OSMA) has recommended that all physicians drop out of the Medicaid program in order to protect themselves from underpayment for their services.
What about the patients otherwise qualified for Medicaid who need health care? OSMA has provided no recommendation. Do the physicians simply refuse to see those patients if they cannot pay cash for their services? Would some physicians agree to see them on a charitable basis at the risk of having their schedules swamped because too many others would continue to boycott the patients until their fee demands were met?
Although we can sympathize with physicians who are being requested to practice in a toxic environment because of unreasonable policy decisions made by the politicians, we can also be troubled by their abandonment of the needy patients who seem to be the real victims here. This is not unlike some members of Congress who have repeatedly voted to repeal the Affordable Care Act yet have offered no replacement to ensure that people can get the health care that they need.
We could replace the politicians who have refused to enact policies that would ensure health care for everyone. Physicians could also replace their medical association delegates with those who follow modern Hippocratic traditions: “I will remember that I remain a member of society, with special obligations to all my fellow human beings, those sound of mind and body as well as the infirm.”
What was it the OSMA president said? “We are fully aware this will create an access-to-care crisis for rural residents, vulnerable seniors, the disabled and the nearly 60 percent of Oklahoma babies born under Medicaid,” but they are left with little other choice than to abandon them. Really?
Update:
It appears that they may receive a reprieve with a new proposal from the state Medicaid agency, but that does not excuse them from the fact that they were willing to abandon their Medicaid patients.
Oklahoma physician leaders vote to abandon Medicaid patients
Oklahoma State Medical Association urges doctors to mull leaving Medicaid over 25 percent rate cut
By Barbara Hoberock
Tulsa World, April 1, 2016Oklahoma State Medical Association leaders have voted unanimously to urge members to consider dropping out of Medicaid.
The association’s executive committee took the unanimous vote on Wednesday following an announcement earlier in the week by the Oklahoma Health Care Authority that Medicaid rates could be cut by as much as 25 percent effective June 1.
For the current fiscal year, the state has seen a deepening revenue failure requiring state-appropriated agencies to make cuts.
“We are fully aware this will create an access-to-care crisis for rural residents, vulnerable seniors, the disabled and the nearly 60 percent of Oklahoma babies born under Medicaid,” said OSMA President Woody Jenkins. “But a 25 percent rate cut, combined with previous cuts that had already been made in recent years, will leave many of our members with little choice.”
He said the association in coming days will be offering guidance on its website for doctors on how to opt out of the Medicaid program.
***
KGOU Update:
The third part of the plan would restore the Medicaid reimbursement rate to 86.5 percent of Medicare. Earlier this week, the Oklahoma Health Care Authority proposed reducing the reimbursement rate to providers by 25 percent as a result of the estimated $1.3 billion general revenue shortfall in the upcoming fiscal year.
http://kgou.org/post/oklahoma-health-care-authority-proposes-plan-insure-more-oklahomans#stream/0
One of the flaws in our fragmented, multi-payer system of financing health care is that low-income patients tend to be lumped into the Medicaid program. Since it is a welfare program serving individuals who do not command much political capital, politicians are more willing to use cuts in Medicaid to balance their budgets than cuts for programs designed to serve the general population such as Medicare and Social Security. What lessons can Oklahoma’s proposed 25 percent cut in Medicaid rates provide for us?
As a welfare program, Medicaid does remain chronically underfunded. As such, access problems occur because of a lack of willing providers since there is reluctance on the part of others to accept the lower Medicaid rates. But should the less fortunate members of society be relegated to a lower standard of health care, or should everyone have the equivalent access to essential health care services? That question has been answered by our politicians even if it was never asked.
That said, what response should organized medicine have to these cuts in Medicaid? Perhaps we should ask whom they perceive as being victimized here. The Oklahoma State Medical Association (OSMA) has recommended that all physicians drop out of the Medicaid program in order to protect themselves from underpayment for their services.
What about the patients otherwise qualified for Medicaid who need health care? OSMA has provided no recommendation. Do the physicians simply refuse to see those patients if they cannot pay cash for their services? Would some physicians agree to see them on a charitable basis at the risk of having their schedules swamped because too many others would continue to boycott the patients until their fee demands were met?
Although we can sympathize with physicians who are being requested to practice in a toxic environment because of unreasonable policy decisions made by the politicians, we can also be troubled by their abandonment of the needy patients who seem to be the real victims here. This is not unlike some members of Congress who have repeatedly voted to repeal the Affordable Care Act yet have offered no replacement to ensure that people can get the health care that they need.
We could replace the politicians who have refused to enact policies that would ensure health care for everyone. Physicians could also replace their medical association delegates with those who follow modern Hippocratic traditions: “I will remember that I remain a member of society, with special obligations to all my fellow human beings, those sound of mind and body as well as the infirm.”
What was it the OSMA president said? “We are fully aware this will create an access-to-care crisis for rural residents, vulnerable seniors, the disabled and the nearly 60 percent of Oklahoma babies born under Medicaid,” but they are left with little other choice than to abandon them. Really?
Update:
It appears that they may receive a reprieve with a new proposal from the state Medicaid agency, but that does not excuse them from the fact that they were willing to abandon their Medicaid patients.
Who isn’t insured, and how can we change that?
Who Are the Remaining Uninsured, and What Do Their Characteristics Tell Us About How to Reach Them?
By Linda J. Blumberg, Michael Karpman, Matthew Buettgens, and Patricia Solleveld
Robert Wood Johnson Foundation
Urban Institute, March 2016
From the Introduction
Although the ACA was not designed to eliminate uninsurance, a detailed assessment of those remaining uninsured after reform can provide insight into the potential to increase coverage further.
Main Findings
* According to the CPS-ASEC, 32.9 million nonelderly residents of the United States remained uninsured as of March 2015, constituting 12.2 percent of the total non-elderly, civilian, non-institutionalized population of the country.
* The rate of uninsurance is significantly higher in (Medicaid) nonexpansion states, where 15.4 percent of the nonelderly are uninsured compared with only 10.1 percent in expansion states, a relative difference of over 50 percent.
* About 28 percent of the uninsured are eligible for Medicaid or the Children’s Health Insurance Program (Medicaid/CHIP), and 21 percent are eligible for marketplace tax credits.
* Fully 66.5 percent of uninsured children are eligible for Medicaid/CHIP compared with only 20.6 percent of uninsured adults.
* We posit that the uninsured who are eligible for the greatest amount of financial assistance under the ACA — 12.4 million uninsured in total — are those for whom additional outreach and enrollment efforts are likely to be most successful.
* Absent further policy changes (e.g., more states expanding Medicaid, increased financial assistance, and expanded eligibility for assistance), we do not expect that a substantial share of the other uninsured — who constitute 20.6 million of the total — will gain coverage.
* Targeting of resources to those 12.4 million uninsured with the greatest potential to enroll in either Medicaid/CHIP or marketplace coverage can be improved by understanding their characteristics.
From the Conclusion
Our analysis of the CPS-ASEC combined with past work on program participation rates and case studies on insurance enrollment behavior under the ACA suggests that two subpopulations of the uninsured have the most promise in further expanding coverage: the Medicaid eligible and the low-income marketplace tax credit eligible. These are the uninsured eligible for the most comprehensive coverage at the lowest direct cost under current law, and those eligible for this level of assistance have relatively high rates of participation in health insurance programs. Together, these subgroups account for 37.5 percent of the remaining uninsured, or approximately 12.4 million people.
Under current law, however, expectations of increasing coverage substantially among the other 62.5 percent of the remaining uninsured should be tempered. Although some additional coverage within these groups is likely as the individual mandate penalties increase and information on available coverage alternatives spread further, gains are likely to be quite modest unless further financial assistance is provided.
http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf427898
***
Comment:
By Don McCanne, M.D.
Perhaps the most important statement in this report on the remaining uninsured is the following: “The ACA was not designed to eliminate uninsurance.” It should be no surprise that we are left with trying to figure out why so many are uninsured and who they are when the architects of the Affordable Care Act abandoned, in advance, any effort to make health care insurance truly universal.
If there is good news in this report it is that there are two groups in which, with concerted effort, we can increase rates of enrollment: the uninsured eligible for Medicaid/CHIP, and the lower-income uninsured eligible for government subsidies for ACA exchange plans. These eligible individuals are more likely to accept coverage because government subsidies make it free or very low cost to them. But those eligible are still a minority of the uninsured – 12.4 million individuals.
The majority of the uninsured – 62.5 percent, 20.6 million individuals – have no publicly-supported programs available for them and are likely to remain uninsured. It has been suggested that we can expand coverage through incremental changes in ACA, but, because of political, logistical and financial barriers, it would be very difficult to design add-on programs that would be effective in bringing these individuals under the coverage umbrella.
Another problem is that a static picture at one point in time does not lead to policies that would address the instability in coverage due to changes in income, employment, age, residency, and other requirements that determine the type of coverage for which an individual may or may not be eligible. As we work on the front end to expand coverage to the currently uninsured, people are falling off of the back end as they lose their coverage and may face new barriers to transitioning to other programs. This instability makes it virtually impossible to ever cover everyone simultaneously under our fragmented system that has been perpetuated by ACA.
So do we want everyone insured? I would say absolutely yes, but it is not going to happen under a system that was clearly not designed to do that. In contrast, an Improved Medicare for All would be designed to actually cover everyone, permanently, not to mention the multitude of other social and health benefits that it would bring to all of us.