http://www.pittsburghlive.com/x/pittsburghtrib/opinion/bish/e_1_2011-06-22.html
Vermont’s health reform law: A five part series
(Vermont’s Super MedPAC, Federal and ERISA plans, Pharma, Anti-trust, and Financing)
By Kevin Outterson, Professor of Law and Health Policy at Boston University
The Incidental Economist on-line, May 6, 2011
H.202 passed the House 94-49 yesterday and Governor Shumlin promises to sign it. The Vermont law deserves some careful attention, but doesn’t appear to be creating much of a stir in Vermont itself – the lead story in this morning’s Burlington Free Press was flooding on Lake Champlain and the most popular story on the website was UVM students in an annual clothing-optional rite of spring.
I’ve read the law (142 pages, a joy by federal standards) and will post throughout next week:
Vermont’s Super MedPAC
While Washington continues to debate the federal IPAB, Vermont has now passed a much more powerful version at the state level, the Green Mountain Care (GMC) Board. Among its powers (18 VSA §9375) are rule making authority that IPAB can only dream about:
Implement by rule, pursuant to 3 V.S.A. chapter 25, methodologies for achieving payment reform and containing costs, which may include the creation of health care professional cost-containment targets, global payments, bundled payments, global budgets, risk-adjusted capitated payments, or other uniform payment methods and amounts for integrated delivery systems, health care professionals, or other provider arrangements.
Notice the absence of exceptions for doctors and hospitals. Rate setting figures prominently:
Set rates for health care professionals [including drugs and devices] pursuant to section 9376 of this title, to be implemented over time, and make adjustments to the rules on reimbursement methodologies as needed.
They also have oversight review for:
- Benefit packages;
- Insurance rate increases;
- Hospital budgets;
- CONs; and
- Quality and performance outcome measures
Fun fact: the Chair of GMC board is paid $116,688 (plus free health care!) (Sec 33a)
Federal and ERISA plans in Vermont’s GMC
Vermont’s single payment system law (Green Mountain Care or GMC) will certainly include all state and municipal employees, everyone in the VT exchange, and individual and small group markets directly regulated by the state.
The law also intends to cover state workers’ compensation injuries – a historic move towards full integration.
For federal entitlement plans – Medicare and Medicaid – Vermont will ask the Obama Administration for waivers so that all of these federal funds are paid directly to Green Mountain Care, with all federal rules waived, including Part D formularies. If these waivers are granted, all Medicare and Medicaid reimbursement rules would be suspended in Vermont and all providers paid solely under GMC.
Other federal plans – TRICARE, VA and FEHBP – are left for another day, as are employees of foreign governments.
The last category includes private ERISA plans, which are shielded from state law to various degrees (fully self-insured plans enjoy the greatest freedom). Vermont can’t force these plans to conform to GMC (as the Supreme Court has made abundantly clear in almost two dozen ERISA opinions), but these employers could voluntarily choose to participate. Vermont is considering a “pay whether or not you play” tax on all employers to fund GMC, which would certainly encourage ERISA plans to either join GMC or leave the state altogether. (One prominent employer in Burlington with a self-insured ERISA plan has put a “for lease” sign up at the local office). The Governor’s job over the next few months is to persuade these employers to voluntarily participate in GMC, with this tax being the stick. The carrot is the promise of a cheaper health care system that actually works.
Bad news for PhRMA in VT
Marjorie Powell is PhRMA’s point person for state legislation. Vermont is one of her problem children – and not just Vermont. States in the northeast seem to love legislation that the drug industry hates. The Maine Rx program was litigated to the Supreme Court back in 2003 (PhRMA v. Walsh), with the drug industry losing 6-3. More recently, the anti-data mining statutes in Maine, New Hampshire and Vermont triggered split decisions in the First and Second Circuits and an appeal to SCOTUS earlier this year. Oral arguments were heard in April.
Part of the story is that the northeast is an incubator for innovative prescription drug policy, supported in no small part by the National Legislative Association on Prescription Drug Pricing (NLARx). Their website is a cornucopia of model legislation and policy papers; what we’d expect from NCSL if it was totally free from drug company influence. (Disclosure: I’ve donated time to NLARx over the years).
Which brings us to Vermont’s single-payment system (GMC). Several items in this law will keep Marjorie and her friend busy. This not a final plan yet, but simply a framework of things drug companies don’t like:
- Evaluate a single state-wide drug formulary – recommendation due by Jan 15, 2012. Expect every drug-company supported patient advocacy group to testify against this. (See the excellent Pro Publica report on PhRMA support to patient advocacy groups). In any event, it is not clear that a single formulary would save money. Much more flexible formulary rules and aggressive generic & therapeutic substitution might. (Health Affairs ungated).
- Dramatically expand use of 340B pricing, potentially for all drugs in GMC. I don’t know how this is possible – 340B was designed for low-income populations, not entire states. Expanding 340B to all eligible populations is a great idea, since the prices are quite low, but making it universal will threaten access for the free clinics that were the historic base for 340B. (I’ve written about price discrimination in prescription drug markets in US Senate testimony and the Yale Journal of Health Policy, Law & Ethics).
- VT may request a full part D waiver, rolling all Part D drug purchasing into GMC. This would bypass the debate on CMS “negotiating” Part D drug prices by letting the state try.
- VT will also consider buying all GMC drugs through Medicaid, with the statutory and supplemental rebates. I don’t know how a state could buy drugs through Medicaid for non-Medicaid populations. This also threatens to undermine the US price disc
rimination scheme. In any event, PhRMA can offset the rebates by raising prices.
- A single mechanism for negotiating rebates and discounts, concentrating and leveraging the state’s buying power, creating a monopsony to negotiate with monopolies.
- Expanding anti-datamining, gift ban, & transparency rules. Not in the legislation at present, but expect it to be added if the Supreme Court strikes down the current version of the VT anti-datamining law in Sorrell v. IMS.
- Importation from Canada. Also missing from the list, but a perennial option frequently discussed in VT.
The state action doctrine under the Vermont single payment system
The Vermont single-payment system legislation requires competitors to work together in a collaborative fashion generally prohibited by federal antitrust laws. The Act protects Vermont providers and others from federal antitrust scrutiny through the “state action” doctrine, which grants antitrust immunity to actions by US states. If a state wants to create monopolies in cable television, toll roads or public utilities, the federal antitrust statutes won’t stand in the way.
Some implications in Vermont:
- Anything the State does directly is immune; and
- Acts by private parties (payers, providers, etc.) may be immune if they are acting pursuant to a clearly articulated state policy and are closely supervised by the State.
18 VSA §9376(d) (§3 of the Act) intentionally provides state action immunity:
(d) To the extent required to avoid federal antitrust violations and in furtherance of the policy identified in subsection (a) of this section, the [GMC] board shall facilitate and supervise the participation of health care professionals and health care provider bargaining groups in the process described in subsection (b) of this section.
Also in §9377(a):
It is also the intent of the general assembly to ensure sufficient state involvement and action in the design and implementation of the payment reform pilot projects described in this section to comply with federal and state antitrust provisions by replacing competition between payers and others with state-supervised cooperation and regulation.
Other similar provisions are in 18 VSA §§9377(c) (§3 of the Act), 18 VSA §724 (§3c of the Act).
Financing the VT single-payment system
H.202 builds the framework for a single-payment system in VT, but doesn’t pull the trigger yet. Two financing plans will be presented to the Legislature by January 15, 2013 (see sec.9). For background, skip the legislation and look at the official report by Hsiao, Kappel and Gruber.
The current model is a payroll tax, on both employers and employees, with exemptions for low-income workers. In fundamental design, this is similar to Social Security or Medicare. The tax rate numbers are not set in stone, but one estimate is 11% for employers and 3% for employees. If Vermont can pay for health care with just 14% of wages, that will be a remarkable bargain.
The tax applies whether or not the employee accepts GMC. This is a “pay whether or not you play” tax – quite different from the “pay or play” laws in Maryland or SF. As a prominent Vermont employer said, no one wants to pay for health care twice, so this structure encourages the self-insured ERISA plans to voluntarily join GMC.
Okma – A European Perspective of U.S. Health Reform
Obama’s Health Reform in European Perspective
By Kieke G. H. Okma
Journal of Health Politics, Policy and Law, June, 2011It is hard to understand the European perspective on the current health reform debate in the United States without calibrating the left-right “scale” of politics in the two continents. If we were to rank political parties in Europe from, say, 1 to 10, the similar scale in America would run from 5 to 15. Thus, Europe’s middle is located at or close to America’s (extreme) left; likewise, America’s far right is way off the European chart. (That also explains why Europeans have a hard time understanding or taking seriously the Tea Party Movement.)
That political convergence of the main political parties in Europe, combined with “corporatist” policy making where governments share the responsibility for social policy making with organized stakeholders, explains why there is much less political polarization than in the United States — particularly on health care issues. European citizens, in the last quarter of the twentieth century, expected and accepted government intervention to make sure everyone has access to health care via state- sponsored or state provided arrangements. They still do. Once in place, welfare programs tend to create their own constituencies. It is hard, politically speaking, to reduce entitlements of existing programs. Even in times of economic downturn and fiscal strains, few European politicians have proposed serious cutbacks in public health spending. Leveling of growth rates of health expenditure, yes, perhaps. Experiments with a modest degree of “markets” based on consumer choice and much government regulation, maybe. But a substantial delisting of entitlements or major increases in user fees are not seriously on the agenda anywhere, especially not when such cuts would affect the elderly or people with chronic illness.
The vast majority of Europeans warmly embraced Obama’s election promise to enact universal health financing. They see universal access to health care as a social right, a crucial element of a decent society.
Two common misperceptions have generated disappointment, however. It is now clear that the 2010 health reform legislation will leave substantial numbers of Americans uninsured. The first error arose from applying the wrong political scale. The U.S. “middle of the road” is much more conservative than that in Europe, and no U.S. president can afford to be seen at the far left of the American scale. The second misunderstanding concerns the power of the American presidency. Surely, Europeans believe, the president of the most powerful country in the world can do what he sets out to do (and surely, no one could be against universal health care either). They find it hard to accept that the president’s power is bound by political institutions that make major change very difficult if not impossible.
The Patient Protection and Affordable Care Act signed by Obama on March 23, 2010, takes on many problems. The health reform law will reduce the number of uninsured by expanding access to Medicaid and imposing restrictions on private insurers (the law also contains many other provisions that only weakly relate to health insurance reform). The step toward universal coverage, however, with effective cost control that would require a form of collective action, was one bridge too far.
Policy is easy. Politics isn’t. For the United States, the politics of collective action on health reform has been one bridge too far. Let’s now build that bridge.
In defense of Canada
By Aaron Carroll
The Incidental Economist, June 5, 2011
Paul Krugman has been on a tear the last few days with a number of posts defending Canada’s Medicare. This was all leading up to his latest column, where he questioned why Medicare should be unsustainable in this country, when it’s sustainable there.
I’m sure we’re going to now face the usual howls of protest, comparing Canada’s health care system to a death sentence. So let me summarize a few of my past posts to try and pre-empt some of the false rhetoric.
1) Doctors in Canada are not flocking to the US to practice

So when emigration “spiked,” 400-500 doctors were leaving Canada for the United States. There are more than 800,000 physicians in the U.S. right now, so I’m skeptical that every doctor knows one of those emigres. But I’d especially like you to pay attention to the yellow line, which is the net loss of doctors to Canada.
In 2003, net emigration became net immigration. Let me say that again. More doctors were moving into Canada than were moving out.
2) Canadians are not flocking here to get care
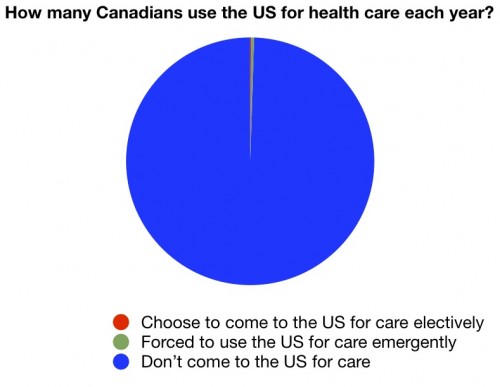
Look, I’m not denying that some people with means might come to the United States for care. If I needed a heart/lung transplant, there’s no place I’d rather be. But for the vast, vast majority of people, that’s not happening. You shouldn’t use the anecdote to describe things at a population level. This study showed you three different methodologies, all with solid rationales behind them, all showing that this meme is mostly apocryphal.
3) Doctors are not less satisfied practicing in Canada than the US
How satisfied are physicians with their practice? It’s not a perfect measure, but it’s an important one:

Given the rhetoric of how much physicians hate reform, you would think doctors were very happy before reform passed. You’d be wrong. With the exception of Austria and Germany, fewer doctors were satisfied with practicing medicine [in the US] than any other surveyed country.
When people want to demonize single payer systems, they always wind up going after rationing, and more often than you’d think with hip replacements…
It’s not true. They don’t deny hip replacements to the elderly. But there’s more.
Do you know who gets most of the hip replacements in the United States? The elderly.
Do you know who pays for care for the elderly in the United States? Medicare.
Do you know what Medicare is? A single-payer system.
5) Canada’s wait times aren’t due to its being a singe-payer system
The wait times that Canada might experience are not caused by its being a single payer system.
Do you know who pays for care for the elderly in the United States? Medicare.
Do you know what Medicare is? A single-payer system.
So our single-payer system manages not to have the wait times issue theirs does. There must be some other reason for the wait times. There is, of course. It’s this:
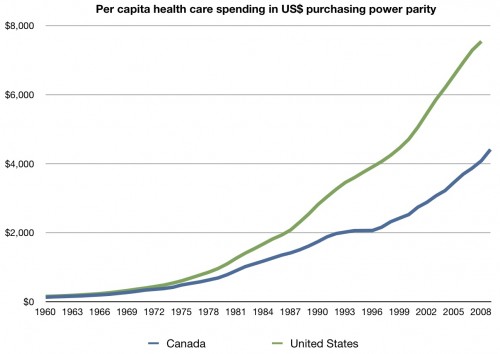
Canada isn’t some dictatorship. They aren’t oppressed. In 1966, the democratically elected government enacted their single-payer health care system (also known as Medicare). Since then, as a country, they have made a conscious decision to hold down costs. One of the ways they do that is by limiting supply, mostly for elective things, which can create wait times. Their outcomes are otherwise comparable to ours.
Please understand, the wait times could be overcome. They could spend more. They don’t want to. We can choose to dislike wait times in principle, but they are a byproduct of Canada’s choice to be fiscally conservative. They chose this. In a rational world, those who are concerned about health care costs and what they mean to the economy might respect that course of action. But instead, we attack.
6) Since Canada adopted their single payer system, infant mortality has dropped below that of the US
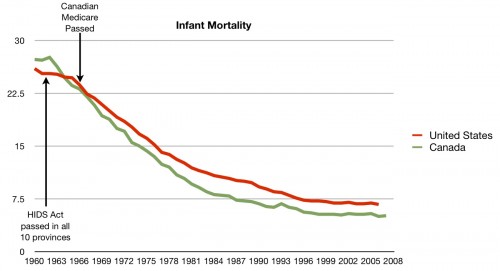
Many people have told me that infant mortality used to be higher in Canada than in the US, but since the passage of (Canadian) Medicare, that hasn’t been the case. The chart above, which I made from OECD data, would tend to agree.
I know the usual knocks against infant mortality as a population metric of quality. But I’d like to hear a good alternate explanation (if one exists) for the trend you see above. Links to evidence or data supporting your theory will get you extra points.

About one third of Americans report that they didn’t go to the doctor when sick, didn’t get recommended care when needed, did not fill
a prescription, or skipped doses of medications in the last year because of cost.
So feel free to have a discussion about the relative merits of the Canadian health care system compared to ours. Just keep it to facts.
http://theincidentaleconomist.com/wordpress/in-defense-of-canada/
Protesters Rally Against Health Insurers
By Katharine Mieszkowski
The Bay Citizen (San Francisco), June 16, 2011
More than 100 protesters from community and labor groups rallied outside the Moscone Center in downtown San Francisco Thursday morning to call for the end of private health insurance and for “Medicare for all,” while members of the America’s Health Insurance Plans met at their national convention inside.
“There is no reason to have a health insurance industry. It only serves them. It doesn’t serve the public,” said Arthur Persyko, a volunteer with Single Payer Now, a San Francisco-based health care reform advocacy group. “They are there to make their bottom line happy. They deny care to people who need it. They are a useless, destructive part of our health care system. It’s a crime, really.”
State Sen. Mark Leno is sponsoring legislation, SB 810, that would establish a universal health care system in California. A similar bill passed the legislature in 2006 and again in 2008, but was vetoed both times by then-Gov. Arnold Schwarzenegger. Advocates say with a Democrat now in the governor’s seat, this time could be different. But even if the bill does ultimately pass, it does not include funding for such a system.
“Separate legislation or a ballot measure would have to finance it,” said Anthony Wright, executive director of Health Access, a consumer advocacy group.
http://www.baycitizen.org/blogs/pulse-of-the-bay/protests-rally-against-health-insurers/
Single-Payer Hopefuls Press Their Cause
By David Gorn
California Healthline, June 17, 2011
Only in San Francisco can a guy wearing a rainbow rasta wig be a voice of reason.
But there he was, among an estimated 400 boisterous protesters, trying to keep the sidewalk clear so pedestrians could pass through the colorful event. Event organizer Don Bechler also was busy keeping the gathering legal and peaceful.
“America deserves a health care system that’s not broken,” said Bechler, chair of California-based Single Payer Now. “We want to get rid of the insurance companies and their bureaucracy of denial. It’s crazy that doctors need to spend so much time dealing with insurance companies — that’s madness to deal with that kind of bureaucracy.”
Health care providers, labor groups and single-payer advocates turned out on the street outside of the annual convention of America’s Health Insurance Plans, a national trade group of health insurers.
Inside, political luminaries addressed the health care insurance industry — from former Senator Tom Daschle, a Democrat from South Dakota, to Republican presidential hopeful and Minnesota Gov. Tim Pawlenty.
Outside, protesters chanted, speakers orated, a pair of giant puppets battled each other (nominally an American citizen taking on insurance groups, but you really had to use your imagination) — and at one point the crowd was treated to the singing of a well-dressed group of ladies who called themselves the Raging Grannies of the Peninsula. They held signs reading “Survival of the Richest” and “Let Them Eat Advil.”
It was good theater, but critical care nurse Bobby Roberts came from San Pablo for more serious reasons.
“I see it all the time, insurers turning down health claims left and right. You see that they’re more worried about profits than patients,” Roberts said. “I have stories and stories, I could go on for days.”
National health care reform is a start, Roberts said, but he’s hoping to one day see the end of health insurance companies altogether. “It’s too much,” he said. “Too much profit, too much paperwork, too many people not getting the care they need. The insurance companies are fleecing us, that’s just so clear.”
Organizers estimated the crowd at about 400 people. San Francisco police reported no complaints.
Single-payer rally ‘welcomes’ insurance industry group
By Marilyn Bechtel
People’s World, June 17, 2011
SAN FRANCISCO – This city is known for its hospitality. So it’s no surprise that this week’s meeting of America’s Health Insurance Plans, the health insurance industry’s national trade association, was greeted by a “welcoming committee.”
But that committee, several hundred strong June 16 on the sidewalk in front of Moscone Center downtown, had a message that AHIP members probably didn’t want to hear.
“Everybody in, nobody out!” they chorused, demanding passage of SB 810, a state single payer-health care bill now before the California legislature, and “Medicare for All” across the nation.
“I’m here today because no one in America should have to worry about whether they can afford health care for themselves or their families,” said California Nurses Association Co-President DeAnn McEwen. “Healthy people are our country’s greatest national resource.”
United Educators of San Francisco President Dennis Kelly galvanized the crowd with his account of the Montana town that, in the wake of a terrible industrial accident, now has single-payer health care for all its residents.
When pollution from an asbestos mine sickened residents of Libby and surrounding areas, Kelly said, Sen. Max Baucus, D-Mont., turned to Medicare. “They declared that the entire town was eligible for Medicare. Because it is single payer, it was the only way to get coverage for absolutely everyone. If Baucus can do that, that’s what we must do in California and the nation.”
(Interestingly, Baucus opposed including single payer in negotiations for last year’s health care reform bill.)
In a statement presented by aide Kim Alvarenga, State Assembly member Tom Ammiano, D-San Francisco, emphasized the importance of covering everyone, including immigrants, documented and undocumented. He said SB 810 “provides universal health care for every single resident of the state … Every person in this country, regardless of race, gender identity, age, disability or legal status has a human right to quality affordable health care.”
Several members of the Chinese Progressive Association’s Youth MOJO (Youth Movement of Justice Organizing) told how losing health coverage has affected them and their families, and described their work for universal health care, immigrant rights and other social justice issues.
Among the speakers and the crowd were members of many unions and community organizations, including the California Alliance for Retired Americans.
The California legislature has previously passed single-payer legislation, only to see it vetoed by former Governor Arnold Schwarzenegger. This year, State Senator Mark Leno, D-San Francisco, introduced SB 810, which has nine cosponsors in the Senate and 20 in the Assembly.
Last month, Vermont Gov. Peter Shumlin, a Democrat who campaigned on the issue, signed a bill taking the first step toward
establishing a statewide single-payer system. In coming years, the legislature will flesh out the program, which is to take effect in 2017.
http://peoplesworld.org/single-payer-rally-welcomes-insurance-industry-group/
‘Medicare for All,’ Activists Tell Insurance Convention
By Jonathan Nack
Indybay.org, June 17, 2011
OAKLAND, Calif. – Protesters greeted the national convention of America’s Health Insurance Plans, held in San Francisco, with their demands for a government run single-payer health care system modeled on Medicare that would cover everyone. The protest took place at Moscone Center in San Francisco, Thursday, June 16, 2011.
Groups participating in the protest included: Single Payer Now, the California Nurses Association, the California Alliance for Retired Americans, Healthcare For All, the S. F. Chinese Progressive Association, the Santa Clara County Single Payer Healthcare Coalition, the Gray Panthers, the Wellstone Democratic Club, and the Alameda County Green Party.
Several photos:
http://www.indybay.org/newsitems/2011/06/17/18682115.php
Man Turns to Crime for Prison Health Care
By ROBERT MACKEY
The Lede Blog, New York Times, June 20, 2011
As if conjured up by a presidential speechwriter to star in an anecdote about America’s dysfunctional health insurance system, James Verone, an unemployed 59-year-old with a bad back, a sore foot and an undiagnosed growth on his chest, limped into a bank in Gastonia, N.C., this month and handed the teller a note, explaining that this was an unarmed robbery, but she’d better turn over $1 and call the cops. That, he figured, would be enough to get himself arrested and sent to prison for a few years, where he could take advantage of the free medical care.
Just to make sure that no one was confused about his intentions, Mr. Verone made sure to let the teller know that he would be sitting on a couch in the bank, waiting for the police. Before he set out for the bank that morning, he also mailed a letter explaining his scheme to a local newspaper, The Gaston Gazette.
“When you receive this a bank robbery will have been committed by me. This robbery is being committed by me for one dollar,” the letter read. “I am of sound mind but not so much sound body.”
In a television interview last week with a local news station, WCNC, Mr. Verone explained that he was hoping for a three-year sentence, which would give him a place to live and free health care until he was old enough to collect a Social Security check and buy a condo on the beach. “I’m sort of a logical person and that was my logic, what I came up with,” he said.
According to Diane Turbyfill, a Gazette journalist who also interviewed Mr. Verone, there was one flaw in his cunning plan. “Because he only demanded $1, he was charged with larceny from a person,” not bank robbery, Ms. Turbyfill wrote. “Still a felony, the count doesn’t carry as much jail time as bank robbery.”
http://thelede.blogs.nytimes.com/2011/06/20/man-turns-to-crime-for-prison-health-care/
AMA 2011 Insurer Report Card
New AMA Health Insurer Report Card Finds Increasing Inaccuracy in Claims Payment
AMA
June 20, 2011
According to the AMA’s latest findings, commercial health insurers have an average claims-processing error rate of 19.3 percent, an increase of two percent compared to last year. The increase in overall inaccuracy represents an extra 3.6 million in erroneous claims payments compared to last year, and added an estimated $1.5 billion in unnecessary administrative costs to the health system. The AMA estimates that eliminating health insurer claim payment errors would save $17 billion.
Physicians received no payment at all from commercial health insurers on nearly 23 percent of claims they submitted. There are many reasons a legitimate claim may go unpaid by an insurer. Claims may be denied, edited or deferred to patients. During Feb. and March of this year, the most common reason insurers didn’t issue a payment was due to deductible requirements that shift payment responsibility to patients until a dollar limit is exceeded.
Metric 6: First ERA accuracy:
This metric measured the percentage of claim lines where the payer’s allowed amount was equal to the physician practice’s expected allowed amount. For this metric, it was necessary to obtain the actual contracted allowed amounts (i.e., fee schedule) for each claim line.
81.08% – Aetna
61.05% – Anthem Blue Cross/Blue Shield
83.02% – CIGNA
87.04% – Health Care Services Corporation
81.99% – Humana
88.41% – Regence
90.23% – UnitedHealthcare
96.19% – Medicare
AMA press release:
http://www.ama-assn.org/ama/pub/news/news/ama-health-insurer-report-card.page
2011 National Health Insurer Report Card:
http://www.ama-assn.org/resources/doc/psa/2011-nhirc-results.pdf
Methodology:
http://www.ama-assn.org/resources/doc/psa/2011-nhirc-methodology.pdf
Comment:
By Don McCanne, MD
The private health insurance industry’s primary product that they are selling us is administrative services. How well are they doing? One-fifth of the claims that they process are in error. Medicare does better, but in using private billing contractors, their claims are still incorrect 4 percent of the time. We’re sure paying a lot to an industry that is doing such a lousy job.
Another finding that is buried in this report is that physicians received no payment at all from commercial health insurers on nearly 23 percent of claims they submitted. Think of the amount of administrative hassle involved here that is producing… nothing! The supposedly legitimate reasons for nonpayment include failure to meet the deductible, insurance policy has been cancelled, employer changed health plans, failure to use a network physician, services are not an included benefit, etc.
Under our current dysfunctional system of financing health care such denied claims are expected, as is the administrative waste entailed. But think of how it would be under a single payer system. None of these would be reasons to deny a claim. With everyone covered under one set of single payer rules, claims payment rate would be close to 100 percent.
Our current health care financing system is highly flawed, and the commercial insurers are incompetent. And we want more of this?!
AMA 2011 Insurer Report Card
New AMA Health Insurer Report Card Finds Increasing Inaccuracy in Claims Payment
AMA
June 20, 2011According to the AMA’s latest findings, commercial health insurers have an average claims-processing error rate of 19.3 percent, an increase of two percent compared to last year. The increase in overall inaccuracy represents an extra 3.6 million in erroneous claims payments compared to last year, and added an estimated $1.5 billion in unnecessary administrative costs to the health system. The AMA estimates that eliminating health insurer claim payment errors would save $17 billion.
Physicians received no payment at all from commercial health insurers on nearly 23 percent of claims they submitted. There are many reasons a legitimate claim may go unpaid by an insurer. Claims may be denied, edited or deferred to patients. During Feb. and March of this year, the most common reason insurers didn’t issue a payment was due to deductible requirements that shift payment responsibility to patients until a dollar limit is exceeded.
Metric 6: First ERA accuracy:
This metric measured the percentage of claim lines where the payer’s allowed amount was equal to the physician practice’s expected allowed amount. For this metric, it was necessary to obtain the actual contracted allowed amounts (i.e., fee schedule) for each claim line.
81.08% – Aetna
61.05% – Anthem Blue Cross/Blue Shield
83.02% – CIGNA
87.04% – Health Care Services Corporation
81.99% – Humana
88.41% – Regence
90.23% – UnitedHealthcare
96.19% – MedicareAMA press release:
http://www.ama-assn.org/ama/pub/news/news/ama-health-insurer-report-card.page2011 National Health Insurer Report Card:
http://www.ama-assn.org/resources/doc/psa/2011-nhirc-results.pdfMethodology:
http://www.ama-assn.org/resources/doc/psa/2011-nhirc-methodology.pdf
The private health insurance industry’s primary product that they are selling us is administrative services. How well are they doing? One-fifth of the claims that they process are in error. Medicare does better, but in using private billing contractors, their claims are still incorrect 4 percent of the time. We’re sure paying a lot to an industry that is doing such a lousy job.
Another finding that is buried in this report is that physicians received no payment at all from commercial health insurers on nearly 23 percent of claims they submitted. Think of the amount of administrative hassle involved here that is producing… nothing! The supposedly legitimate reasons for nonpayment include failure to meet the deductible, insurance policy has been cancelled, employer changed health plans, failure to use a network physician, services are not an included benefit, etc.
Under our current dysfunctional system of financing health care such denied claims are expected, as is the administrative waste entailed. But think of how it would be under a single payer system. None of these would be reasons to deny a claim. With everyone covered under one set of single payer rules, claims payment rate would be close to 100 percent.
Our current health care financing system is highly flawed, and the commercial insurers are incompetent. And we want more of this?!
"Financial toxicity" of cancer, and AHRQ's Effective Health Care Program
Oncologists confront "financial toxicity" of cancer care
By Pamela Lewis Dolan
American Medical News, June 20, 2011
The toxicity of chemotherapy and other drug treatments for cancer has extended beyond side effects such as nausea and nerve pain. It has now extended to a patient’s ability to pay the mortgage and buy groceries while undergoing care, said the author of a study looking at the financial impact of cancer treatment.
Amy Abernethy, MD, associate professor in the Division of Medical Oncology at Duke University Medical Center, helped write one of a handful of studies presented at the June meeting of the American Society of Clinical Oncology that found the rising cost of cancer care could impact treatment decisions and even lead to patients forgoing treatment because they cannot afford it.
The growing financial burden on those undergoing cancer treatment could put physicians in the position of prescribing treatments that could save their patients’ lives but force them into bankruptcy, poverty or even homelessness — if they could scrape up the money to receive the treatment in the first place. This is especially troubling given the fact that advancements are being made in cancer treatments that could lead to much higher survival rates.
Another study presented at the ASCO meeting was published online June 5 in The New England Journal of Medicine. It found that the experimental drug vemurafenib and the newly approved Yervoy (ipilimumab) can improve survival rates for patients with advanced melanoma, a population that hasn’t had many treatment options in the past. Yervoy will cost $120,000 for a four-dose treatment at $30,000 per dose.
“The move toward increased cost-sharing in high-deductible health plans, increased premiums and tiered formularies all shift the cost burden to patients and force them to make day-to-day decisions on how to integrate health care costs with other discretionary spending,” said (Neal Meropol, MD, chief of the Division of Hematology and Oncology at Case Western Reserve University School of Medicine).
A study conducted by researchers at the Fred Hutchinson Cancer Research Center in Seattle found that as cancer patients’ survival time increases, so do the chances they will declare bankruptcy. Researchers compared U.S. Bankruptcy Court records to cancer registry data from nearly 232,000 adult cancer survivors in western Washington over 14 years. They found that, on average, bankruptcy rates quadrupled within five years of a cancer diagnosis.
http://www.ama-assn.org/amednews/2011/06/20/bil20620.htm
And…
Effective Health Care Program
Agency for Healthcare Research and Quality
The Effective Health Care (EHC) Program partners with networks of researchers and clinical teams across North America, using input from stakeholders throughout the process of comparative effectiveness research, translation, dissemination, and implementation of research findings.
In 2010, AHRQ used funding from the American Recovery and Reinvestment Act of 2009 (ARRA) to establish two important Program initiatives:
* Community Forum to improve and expand public and stakeholder engagement in AHRQ’s comparative effectiveness research and EHC Program.
* Healthcare Horizon Scanning System to identify new and emerging issues for comparative effectiveness review investments.
These initiatives contribute to the work of these Program components:
* Individual investigators and their research groups at academic institutions and other research centers generate new evidence from original research.
* The Evidence-based Practice Centers (EPCs) perform in depth reviews of existing evidence.
* The DEcIDE (Developing Evidence to Inform Decisions about Effectiveness) Research Network gathers new knowledge on specific treatments and health care services.
* The Centers for Education & Research on Therapeutics (CERTs) conduct research and educate clinicians and consumers about drugs, biologicals, and medical devices.
* The Scientific Resource Center provides scientific support for the EHC Program.
* The John M. Eisenberg Center for Clinical Decisions and Communications Science organizes the research results into guides and tools that are useful to clinicians, health care policymakers, and patients.
* The Stakeholder Group provides different perspectives on the EHC Program from individual members of the Group.
http://effectivehealthcare.ahrq.gov/index.cfm/who-is-involved-in-the-effective-health-care-program1/
Comment:
By Don McCanne, MD
Having cancer and facing the agony of treatment is bad enough without also having to face the financial burdens of treatment. As this and many other reports show, “financial toxicity” can seriously impair the ability to meet other basic needs, and may even result in personal bankruptcy.
We do need some reassurance that the costs and adverse effects of the treatments are worth the benefits provided. We shouldn’t use as our sole source of information an industry that might be reluctant to communicate the full downside of their treatments when that information might reduce their very lucrative profits.
Fortunately, we do have a good start on becoming more informed in our choices for health care. The Effective Health Care Program of the Agency for Healthcare Research and Quality (AHRQ) is providing us with comparative effectiveness and evidence-based research that can be very useful in our clinical decision making. However, we do need to move further forward and use this information to make coverage decisions, certainly to eliminate coverage of detrimental health care, and also to eliminate coverage of care that the overwhelming preponderance of information reveals is not beneficial.
We also need to negotiate the best pricing based on legitimate costs and fair profits, and begin to make decisions on tolerance thresholds for health care payments. Everyone would agree that we can’t use our collective funds to pay say $10 million for a treatment program that would extend the life of one person by three weeks, but with the very high prices that are being introduced, we will have to begin to struggle with cost-effectiveness determinations at levels that we find to be tolerable.
Once we are armed with the very best information, we should use that to obtain the highest quality care that’s feasible for each and every individual with health care needs. We should eliminate “financial toxicity” by providing first dollar coverage for not just cancer patients but for all patients who already have enough burdens heaped upon them without having to face onerous financial burdens as well.
Considering a single-payer model for health reform
By Aldebra Schroll, M.D.
KevinMD.com blog at MedPage Today, June 17, 2011
The Patient Protection and Affordable Care Act is in the process of being rolled out, however many questions remain.
Will it guarantee universal coverage? Will it stand up to the many court challenges? The private insurance industry will receive an estimated 400 billion in taxpayer money to subsidize the purchase of these plans. Is this the best way to spend our money?
Many of us in the health field remain skeptical of the program. The Physicians for a National Health Program estimate that approximately 23 million people will remain uninsured. Many more will find themselves underinsured with high co-payments and deductibles. They will have insurance coverage that still leaves them at risk of financial ruin in the event of serious illness. Medical expenses are now a leading cause for personal bankruptcy, often occurring in families that have health insurance. It simply does not offer them adequate coverage.
America spends $2.4 trillion a year on our health care expenditures, more than any other advanced country. Yet this higher spending does not translate into better health status. Americans have a lower life expectancy, higher infant mortality and poorer access to care when compared to most industrialized nations. In a 2002 report, the Institute of Medicine estimated that eighteen thousand patients die annually due to a lack of health insurance.
Where does all the money go? The private insurance health plans consume approximately thirty percent of their expense in administrative costs, profits and CEO salaries. These costs do not directly benefit the patients, instead keeping insurance unaffordable for many Americans.
One reform proposal gaining momentum across the nation is single payer health. Vermont recently passed a single-payer plan after their legislature commissioned Harvard economist Dr. William Hsiao. His analysis determined that a single-payer model would be 25 percent cheaper than continuing the current model that depends heavily on private insurers. In signing the bill, Vermont Governor Peter Shumlin emphasized health care as a right, not a privilege; a feeling shared by many of us working in the front lines of health care.
Under a single-payer plan, physicians and other health care institutions would operate independently and collect payments from a single entity, which would significantly reduce the expense and challenges of collecting from a variety of payers. It would also reduce the administrative costs and the profits that motivate major insurers.
This model was not seriously considered during the national health reform discussions. The tide is turning however; recent surveys of physicians have found 59 percent favor a national health insurance plan. As we continue to move forward on the path of reform, it is crucial we understand where we have been and consider all our options, including the single payer model.
Aldebra Schroll is a family physician.
http://www.kevinmd.com/blog/2011/06/single-payer-model-health-reform.html
Single-payer coverage eyed in New York State
By Douglas Turner
The Buffalo News, June 20, 2011
WASHINGTON — Conservative House Republicans, flush from their 2010 victory over the perceived overreach of the Obama health care law, flooded the Capitol with heroic-sounding legislation last winter.
The titles include the No Taxpayer Funding for Abortion Act, the Reclaiming Individual Liberty Act and my favorite, the Revoke Excessive Policies that Encroach on Individual Freedom Act. There are scores of these ideological bills, most written by health insurance lobbyists or special interest groups. None will become law this session because of the Democratic-controlled Senate and President Obama.
Momentum is moving in a very different direction in liberal Vermont, and maybe in New York State. A month ago, Vermont Gov. Peter Shumlin signed a law that will create a single-payer health care system, parallel to Canada’s.
In New York, Assemblyman Richard Gottfried, D-Manhattan, has introduced legislation creating a single-payer plan for all residents of the state. Gottfried is Health Committee chairman. His bill has more than 60 Assembly and Senate co-sponsors. Among them are Democratic Assembly Members Sam Hoyt, Crystal Peoples-Stokes and Mark F. Schroeder, of Buffalo.
The bill creates the State Health Plan, which would become an authority, drawing revenues from the State Health Trust Fund. The fund would get its money from federal and other funds already going to the state from Medicaid and other sources, plus new payroll taxes. The payroll taxes would be 2 percent on employees, 8 percent on employers and 10 percent on the self-employed. Private health insurance premiums now are about 22 percent to 25 percent of payroll.
New York and Vermont have this in common — both states have a much higher share of their residents covered by either Medicare or Medicaid. In New York, it’s 41 percent and in Vermont, it’s 43 percent, according to the Kaiser Family Foundation. Nationally, the number is 34 percent. The Kaiser data is two years old, so the percentages of public coverage are probably much higher now.
“We can get better coverage, get all of us covered and save billions by having New York provide publicly sponsored single-payer health coverage,” Gottfried said.
He said this may be the closest New York could get to an economic silver bullet, making the state much more “job friendly” by eliminating the need for employers to pay for health insurance.
Right now, the state is in the cellar as a place to do business. Health care costs are at least 16 percent of all goods and services produced statewide, or nationally. Most other industrialized nations spend 8 percent to 10 percent on health care and get better quality.
More importantly, a single-payer system would provide coverage for individuals, as more and more private employers say they are planning to end paying for this defined benefit when the weaker federal plan becomes effective in 2014.
Gottfried’s bill has miles to go before becoming law.Gov. Andrew M. Cuomo has no known position on it. Cuomo was by turns friendly and critical of the insurance industry as attorney general. The bill at least has early strong support from some Democrats from across the state.
In Congress, most Democrats are scared to death of the term “single-payer.” This is because of the propaganda blanket the insurance industry has spread over Washington, huge amounts the health business invests in elections, and the infiltration of ultra-rightists into the national tea party movement.
The Commonwealth Fund notes that Sen. Bernie Sanders, IVt., has a bill calling on all states to create a single-payer system. It has no co-sponsors. Only veteran Rep. John Conyers, D-Mich., has introduced a comprehensive federal single-payer bill called Medicare for All. Among the 60 co-sponsors of the bill, six are from New York; but none from Erie-Niagara.
dturner@buffnews.com
http://www.buffalonews.com/editorial-page/columns/douglas-turner/article460758.ece
“Financial toxicity” of cancer, and AHRQ’s Effective Health Care Program
Oncologists confront “financial toxicity” of cancer care
By Pamela Lewis Dolan
American Medical News, June 20, 2011The toxicity of chemotherapy and other drug treatments for cancer has extended beyond side effects such as nausea and nerve pain. It has now extended to a patient’s ability to pay the mortgage and buy groceries while undergoing care, said the author of a study looking at the financial impact of cancer treatment.
Amy Abernethy, MD, associate professor in the Division of Medical Oncology at Duke University Medical Center, helped write one of a handful of studies presented at the June meeting of the American Society of Clinical Oncology that found the rising cost of cancer care could impact treatment decisions and even lead to patients forgoing treatment because they cannot afford it.
The growing financial burden on those undergoing cancer treatment could put physicians in the position of prescribing treatments that could save their patients’ lives but force them into bankruptcy, poverty or even homelessness — if they could scrape up the money to receive the treatment in the first place. This is especially troubling given the fact that advancements are being made in cancer treatments that could lead to much higher survival rates.
Another study presented at the ASCO meeting was published online June 5 in The New England Journal of Medicine. It found that the experimental drug vemurafenib and the newly approved Yervoy (ipilimumab) can improve survival rates for patients with advanced melanoma, a population that hasn’t had many treatment options in the past. Yervoy will cost $120,000 for a four-dose treatment at $30,000 per dose.
“The move toward increased cost-sharing in high-deductible health plans, increased premiums and tiered formularies all shift the cost burden to patients and force them to make day-to-day decisions on how to integrate health care costs with other discretionary spending,” said (Neal Meropol, MD, chief of the Division of Hematology and Oncology at Case Western Reserve University School of Medicine).
A study conducted by researchers at the Fred Hutchinson Cancer Research Center in Seattle found that as cancer patients’ survival time increases, so do the chances they will declare bankruptcy. Researchers compared U.S. Bankruptcy Court records to cancer registry data from nearly 232,000 adult cancer survivors in western Washington over 14 years. They found that, on average, bankruptcy rates quadrupled within five years of a cancer diagnosis.
And…
Effective Health Care Program
Agency for Healthcare Research and Quality
The Effective Health Care (EHC) Program partners with networks of researchers and clinical teams across North America, using input from stakeholders throughout the process of comparative effectiveness research, translation, dissemination, and implementation of research findings.
In 2010, AHRQ used funding from the American Recovery and Reinvestment Act of 2009 (ARRA) to establish two important Program initiatives:
* Community Forum to improve and expand public and stakeholder engagement in AHRQ’s comparative effectiveness research and EHC Program.
* Healthcare Horizon Scanning System to identify new and emerging issues for comparative effectiveness review investments.These initiatives contribute to the work of these Program components:
* Individual investigators and their research groups at academic institutions and other research centers generate new evidence from original research.
* The Evidence-based Practice Centers (EPCs) perform in depth reviews of existing evidence.
* The DEcIDE (Developing Evidence to Inform Decisions about Effectiveness) Research Network gathers new knowledge on specific treatments and health care services.
* The Centers for Education & Research on Therapeutics (CERTs) conduct research and educate clinicians and consumers about drugs, biologicals, and medical devices.
* The Scientific Resource Center provides scientific support for the EHC Program.
* The John M. Eisenberg Center for Clinical Decisions and Communications Science organizes the research results into guides and tools that are useful to clinicians, health care policymakers, and patients.
* The Stakeholder Group provides different perspectives on the EHC Program from individual members of the Group.http://effectivehealthcare.ahrq.gov/index.cfm/who-is-involved-in-the-effective-health-care-program1/
Having cancer and facing the agony of treatment is bad enough without also having to face the financial burdens of treatment. As this and many other reports show, “financial toxicity” can seriously impair the ability to meet other basic needs, and may even result in personal bankruptcy.
We do need some reassurance that the costs and adverse effects of the treatments are worth the benefits provided. We shouldn’t use as our sole source of information an industry that might be reluctant to communicate the full downside of their treatments when that information might reduce their very lucrative profits.
Fortunately, we do have a good start on becoming more informed in our choices for health care. The Effective Health Care Program of the Agency for Healthcare Research and Quality (AHRQ) is providing us with comparative effectiveness and evidence-based research that can be very useful in our clinical decision making. However, we do need to move further forward and use this information to make coverage decisions, certainly to eliminate coverage of detrimental health care, and also to eliminate coverage of care that the overwhelming preponderance of information reveals is not beneficial.
We also need to negotiate the best pricing based on legitimate costs and fair profits, and begin to make decisions on tolerance thresholds for health care payments. Everyone would agree that we can’t use our collective funds to pay say $10 million for a treatment program that would extend the life of one person by three weeks, but with the very high prices that are being introduced, we will have to begin to struggle with cost-effectiveness determinations at levels that we find to be tolerable.
Once we are armed with the very best information, we should use that to obtain the highest quality care that’s feasible for each and every individual with health care needs. We should eliminate “financial toxicity” by providing first dollar coverage for not just cancer patients but for all patients who already have enough burdens heaped upon them without having to face onerous financial burdens as well.