Table of contents
Click the links below to jump to different sections of the newsletter. To view a PDF version of the shorter print edition of the newsletter, click HERE.
If you wish to support PNHP’s outreach and education efforts with a financial contribution, click HERE.
If you have feedback about the newsletter, email info@pnhp.org.
PNHP News and Tools for Advocates
- Welcome letter from PNHP’s new president, Dr. Diljeet Singh
- “Shadow Hearing” for Dr. Mehmet Oz
- PNHP’s Moral Injury Project receives IRB approval
- Medicare “Advantage” report to measure racial inequities in MA
- Bringing our fight to Washington
Save the Date for our Annual Meeting in Washington, D.C.
Data Update: Health Care Crisis by the Numbers
PNHP Chapter Reports
SNaHP Chapter Reports
- SNaHP Rising (Western University)
- Florida SNaHP
- FSU (Florida State University)
- Health Care for All (Chicago College of Osteopathic Medicine)
- Northwestern SNaHP
- University of Illinois College of Medicine – Peoria
- Iowa SNaHP
- KYCOM (University of Pikeville – Kentucky College of Osteopathic Medicine)
- WMed SNaHP
- Creighton SNaHP
- Jacobs SNaHP
- SNaHP at NEOMED (Northeast Ohio Medical University)
- DUCOM (Drexel University College of Medicine)
- SKMC (Sidney Kimmel Medical College)
Responding to the UnitedHealthcare CEO Murder
PNHP in the News
PNHP News and Tools for Advocates
Welcome letter from PNHP’s new president, Dr. Diljeet Singh

With appalling health outcomes, deplorable health inequities, and staggering rates of medical bankruptcy, we have long known American health care has been broken by an unregulated, profit-driven health insurance industry that must be dismantled. Since taking office, the Trump administration has taken us in the opposite direction. They have begun the destruction of our medical research and public health infrastructure while simultaneously threatening the foundations of traditional Medicare and Medicaid.
At PNHP, we know the fight for health justice is a long one—but we take strength from our growing coalition, and from members like you, who continue to speak out and organize for a truly equitable health care system. We have hope and deep gratitude for all our members engaged with the movement and working to support the well-being of all.
We are especially proud to congratulate our graduating SNaHP (soon to be PNHP!) members who have matched in various specialties across the country. In them, we see the future of our profession: bold, principled, and committed to transforming the system. We are grateful for their co-leadership in our organizing efforts and are excited to support them through their residencies and fellowships.
As we continue building power within our movement, we want to share a few highlights from what we’ve been working on this year: Our Moral Injury Project continues to shine a light on how profit-driven “care” harms both patients and health professionals, our Equity Project is exploring how privatized Medicare plans exacerbate racial inequities, and our legislative advocacy has been in full force, with PNHP members organizing 45 legislative visits, calling for action against corporate abuse, overpayments, and care denials.
Our work does not happen in isolation—we are constantly collaborating with allied organizations to build collective power and push for systemic change. One powerful example was the recent Dr. Oz “shadow hearing,” which we co-hosted with Social Security Works and which was co-sponsored by 12 other organizations. This event spotlighted the devastating harms of corporate health care and amplified the voices of patients, providers, and advocates demanding a better system.
Working together makes us stronger—and brings us closer to the just and equitable health care system we all deserve. That spirit of collaboration and collective action will be front and center at PNHP’s Annual Meeting in Washington, D.C. on Nov. 1-3. We’ll dig deeper into our campaigns to challenge Medicare privatization and strategize together on how to grow our movement in the year ahead.
Thank you so much for your membership, your engagement, and your strength during these politically turbulent times. We are proud to be in this movement with you. Please reach out if I can help support you in any way.
“Shadow Hearing” for Dr. Mehmet Oz
On Friday, March 14, at 9:00 a.m. Eastern—one hour before Mehmet Oz’s official hearing in Washington, D.C.—PNHP hosted a virtual “shadow hearing” to expose the truth about his plans for CMS: Medicaid cuts, Medicare privatization, and the devastating consequences of Medicare Advantage (MA). This event, which was co-sponsored by 13 allied health justice organizations, featured 11 speakers who shared firsthand experiences of the harm caused by privatized health care, whether as patients struggling to access care or as providers fighting insurance denials.
Social Security Works executive director Alex Lawson and PNHP board member Dr. Alankrita Olson joined us live from outside the hearing room in D.C., offering real-time updates on the scene. Together, we worked to counter the pro-privatization narrative pushed by Dr. Oz, whose self-serving perspective disregards the health and well-being of the American people.
The speakers underscored the dangerous reality of so-called “Advantage” plans, which systematically deny care to boost corporate profits, leaving patients in medical and financial distress. Stories highlighted insurers’ routine delays and denials, the administrative burdens placed on providers, and the real-life consequences for those trapped in a system designed to prioritize profits over patients.
This event served as a direct call to action, urging Americans to contact their legislators and demand that they reject policies that would further entrench the privatization of our public health programs.
To learn more about actions you can take today, visit pnhp.org/Oz.
PNHP’s Moral Injury Project receives IRB approval

The PNHP Moral Injury Project has officially received Institutional Review Board (IRB) approval, and we are moving forward with full-scale research and outreach efforts! Since January 2025, our working group of 25 PNHP members and SNaHP students has been meeting regularly, organizing into four dedicated teams to advance different aspects of the project.
The Presentations Team is focused on developing and delivering presentations on moral injury at PNHP chapter meetings, medical society events, and residency programs to raise awareness and spark discussion. The Materials Team is creating essential outreach materials, including an FAQ sheet, flyers, an information sheet, and an outreach toolkit, equipping members with the necessary resources to educate and engage others. (All of these materials can be found at pnhp.org/MoralInjury.) The Research Team is exploring nontraditional research strategies, such as social media outreach, to expand the project’s visibility and impact. Finally, the Network Outreach Team is working to establish connections with medical societies and residency programs to distribute our survey and link the Presentations Team with opportunities to present.
We are also advancing into the second phase of our interviews, where we are designing guides and structuring physician interviews to gather firsthand accounts of moral injury in U.S. health care. Our first round of physician interviews are anticipated to be conducted by the end of April 2025.
If you would like to be involved in our Moral Injury Working Group, please contact Rebecca Delay at rebecca@pnhp.org. Stay tuned for further updates as we expand our outreach, research, and advocacy efforts!
PNHP’s Moral Injury Project is funded with generous support from the Robert Wood Johnson Foundation.
Medicare “Advantage” report to measure racial inequities in MA
PNHP’s Medicare Advantage Equity Project is well underway, focusing on developing a comprehensive report analyzing the impact of MA on racial health inequities. This project seeks to examine and debunk insurers’ claims that their privatized Medicare plans promote health equity, equipping legislators with the information to challenge misleading narratives used to justify MA’s expansion. This project will strengthen PNHP’s advocacy by ensuring policymakers have access to credible research and critical stakeholder insights that expose the harm that corporate insurers inflict on marginalized communities.
To guide this project, we have established two advisory bodies. An internal advisory committee of eight PNHP and SNaHP members is helping shape the research process and ensure validity in our analysis. Additionally, an external steering committee of seven health equity experts from various organizations is advising on research practices, guiding our focus areas, and structuring a framework to align with the project’s mission. Their expertise ensures that our research remains thorough, relevant, and impactful.
So far, we have conducted a literature review exploring existing research on health outcomes for marginalized communities with heavy enrollment in MA plans. This review has helped us identify gaps in current research and begin structuring the framework for our report and the next phase of research. Moving forward, we are working to build upon these findings to present a clear, evidence-based critique of insurers’ equity claims while developing accessible materials for legislators and policymakers. As we continue, our goal remains clear: to expose how MA exacerbates racial health inequities and provide lawmakers with the resources needed to push back against privatization efforts that disproportionately harm vulnerable communities.
Bringing our fight to Washington

On March 27, Rep. Pramila Jayapal sent a letter to the Department of Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS), urging them to take action to curb waste, abuse, and patient harm in Medicare Advantage (MA).
The letter calls for eliminating waste and abuse by improving risk adjustment calculations in the proposed 2026 Medicare Advantage Rate Notice, strictly enforcing overpayment regulations outlined in the 2025 Medicare Physician Fee Schedule rule, and strengthening enforcement against MA insurers that illegally deny care.The letter also calls for reforms to promote health equity by addressing disparities in care outcomes and improving data-sharing mechanisms to help enrollees make informed choices.
PNHP has been actively engaging legislators on this issue, having conducted 45 legislative visits to urge lawmakers to sign onto this letter. Our efforts built on last year’s success, when PNHP’s advocacy helped CMS stand firm against aggressive industry opposition to a more reasonable 2024 MA rate hike. By mobilizing our network to support actuarially sound rate adjustments, we helped counter the immense lobbying power of corporate insurers.
While the political landscape may be more challenging in 2025, PNHP’s advocacy has proven highly effective, and continued mobilization is essential to holding CMS and HHS accountable. Our members are off to an impressive start this year; Rep. Jayapal’s pro-Medicare letter was signed by 78 members of the U.S. House of Representatives, compared to 65 who signed a similar letter in 2024.
Looking ahead, we are anticipating the introduction of the Medicare for All Act in April. Reps. Jayapal and Dingell will be sponsoring the House bill while Sen. Bernie Sanders sponsors the Senate bill. As with previous versions, this legislation would establish a single-payer national health program, removing the profit-driven middlemen that exploit both patients and providers.
PNHP and our allies are already working to urge legislators to sign on as co-sponsors once the bill is introduced. We encourage all PNHP members and supporters to join this effort by contacting their legislators after the bill’s launch and either thanking them for co-sponsoring or urging them to get on board. As we continue to expose the failures of privatized health care and fight back against industry influence, Medicare for All remains the ultimate solution to our nation’s health care crisis. Our advocacy has already made a significant impact, and with strong grassroots mobilization, we can continue to push for fundamental reform.
Save the Date for our Annual Meeting in Washington, D.C.

PNHP’s 2025 Annual Meeting is set for November 1-3 in Washington, D.C., bringing together physicians, medical students, and health care advocates for a powerful weekend of education and action! The weekend will kick off with the SNaHP Summit on Saturday morning, providing medical students with a dedicated space to strategize, connect, and strengthen their organizing efforts.
The PNHP Annual Meeting will begin Saturday afternoon and continue through Monday, featuring panels, discussions, and opportunities to deepen our advocacy for single-payer health care. The event will culminate in a Lobby Day and Rally at the Capitol on Monday, November 3, where members will demand action to protect and expand Medicare while pushing for a single-payer system.
Stay tuned for more details on programming, speakers, and registration!
Data Update: Health Care Crisis by the Numbers
Corporate Profiteering
OIG: Insurers Should Pay Feds Millions: A new watchdog audit found that Humana and CVS Medicare Advantage plans owe the federal government $11 million in overpayments. The HHS Office of the Inspector General (OIG) audited medical claims from 2017-2018 and determined that 202 out of 240 reviewed diagnostic codes from Humana were unsupported by medical records, leading to an estimated $6.8 million in overpayments. Similarly, HealthAssurance Pennsylvania, a CVS subsidiary, had 222 out of 269 diagnostic codes lacking proper documentation, resulting in $657,744 in overpayments. The audit will be sent to CMS officials, who will decide whether to recoup the overpayments. The findings highlight ongoing scrutiny of Medicare Advantage plans and concerns that private insurers are overpaid by CMS. “Feds seek $11M refund from Humana, CVS,” Politico, September 26, 2024.
Report Reveals Billions in Excess Medicare Payments: A new inspector general’s report found that private Medicare insurers received approximately $4.2 billion in extra federal payments in 2023 for diagnoses obtained through company-initiated home visits—many of which did not lead to treatment. These diagnoses, including potentially inaccurate ones, triggered higher payments because Medicare Advantage insurers receive increased reimbursements when patients are classified with costly conditions. The findings raise concerns about how home visits are used to inflate payments without providing meaningful medical care. “Medicare Paid Insurers Billions for Questionable Home Diagnoses, Watchdog Finds,” The Wall Street Journal, October 24, 2024.
Medicare Advantage Denied 1.5 Million Claims in a Single Year, Leaving Patients Vulnerable: In 2019 alone, Medicare Advantage insurers denied 1.5 million claims—18% of all payments—even when they met Medicare coverage rules. These denials force enrollees to either forgo needed medical care or pay out-of-pocket. In 2024, the government will give private insurers an additional $64 billion to cover “free” benefits like dental and vision, yet insurers refuse to disclose how much they actually spend on patient care. A study found that only 11% of enrollees used dental benefits, while another found that a quarter never used any of the advertised perks. Meanwhile, major hospitals like Scripps Health and Mayo Clinic are rejecting Medicare Advantage patients due to unpaid bills. “The Medicare Advantage Trap: What They Don’t Tell You,” The Hartmann Report, October 5, 2024.
Private Medicare Plans Collected $7.5 Billion in Questionable Payments: A new report from the HHS Office of Inspector General (OIG) reveals that private Medicare Advantage plans received $7.5 billion in enhanced payments in 2023 based on potentially suspect patient diagnoses. Most of these risk-adjusted payments came from in-home “health risk assessments” and chart reviews—evaluations often conducted by individuals with no direct involvement in a patient’s care. UnitedHealth Group alone collected over $3.7 billion from these assessments, while Humana received nearly $1.71 billion and Cigna Group took in $237 million. The OIG is calling for greater oversight of these practices to ensure Medicare Advantage insurers are not inflating payments without providing necessary follow-up care. “Watchdog Flags $7.5 Billion Paid to Private Medicare Plans,” Bloomberg Law, October 24, 2024.
Barriers to Care
80% of Mental Health Providers in Medicare Advantage Directories Are Unreachable: A Senate Finance Committee investigation found that Medicare Advantage (MA) plan directories are riddled with “ghost networks,” where listed mental health providers are often inaccurate, unavailable, or out-of-network. In a secret shopper study across six states, staff contacted 120 listed providers and found that 33% had incorrect or non-working numbers, while appointments could only be scheduled 18% of the time. In some states, the success rate was as low as 0%. The report highlights the serious barriers individuals face when seeking mental health care and calls on CMS to strengthen oversight of MA provider directories. It also urges Congress to mandate stricter accuracy requirements, transparency measures, and financial penalties for non-compliance. “Majority Study Findings: Medicare Advantage Plan Directories Haunted by Ghost Networks,” Senate Finance Committee, May 3, 2023.
Medicare Advantage Insurers Deny Critical Post-Acute Care at Alarming Rates: A U.S. Senate investigation found that UnitedHealthcare, Humana, and CVS—covering nearly 60% of Medicare Advantage enrollees—used prior authorization to deny critical post-acute care at disproportionately high rates. In 2022, UnitedHealthcare and CVS denied prior authorization for post-acute care at three times their overall denial rates, while Humana’s denial rate for such care was 16 times higher than its overall rate. UnitedHealthcare’s denials for skilled nursing facilities surged ninefold between 2019 and 2022, while CVS “saved” over $660 million in a single year by denying inpatient care requests. Internal documents show insurers used automation and predictive algorithms to increase denial rates, prioritizing financial savings over medical necessity. “Refusal of Recovery: How Medicare Advantage Insurers Have Denied Patients Access to Post-Acute Care,” U.S. Senate Permanent Subcommittee on Investigations, October 17, 2024.
Prior Authorization Delays Linked to Severe Patient Harm, Physicians Report: A 2024 AMA survey found that 29% of physicians reported prior authorization (PA) has led to a serious adverse event for a patient in their care. Additionally, 23% said PA resulted in a patient’s hospitalization, 18% reported it caused a life-threatening event or required intervention to prevent permanent harm, and 8% stated that PA led to disability, permanent bodily damage, congenital anomalies, or even death. The findings highlight the significant risks PA policies pose to patient safety and the urgent need for reform. “2024 AMA Prior Authorization Physician Survey,” AMA, June 18, 2024.
Medicare Advantage Delays and Denials Worsen Rural Health Care Challenges: A report from the American Hospital Association found that 81% of rural clinicians say insurer requirements under Medicare Advantage (MA) reduce the quality of care, while MA patients experience 9.6% longer hospital stays before receiving post-acute care compared to traditional Medicare patients. Administrative burdens have also intensified, with nearly 80% of rural clinicians reporting increased paperwork over the past five years, and 86% stating that these challenges negatively affect patient outcomes. Delayed or denied MA payments further strain rural hospitals’ finances, threatening access to care in underserved areas. “The Growing Impact of Medicare Advantage on Rural Hospitals Across America,” American Hospital Association, February 2025.
Private Insurance and Medicare Advantage Have Higher Claim Denial Rates Than Traditional Medicare: An analysis found that 21% of people with employer-sponsored insurance and 20% of those with marketplace insurance experienced denied claims, compared to 10% of Medicare beneficiaries and 12% of Medicaid enrollees. A separate 2024 survey of hospitals and post-acute care providers by Premier, Inc. found that nearly 15% of medical claims submitted to private insurers were initially denied, with Medicare Advantage having a higher denial rate of 15.7%. “Breaking Down Claim Denial Rates by Healthcare Payer,” TechTarget, January 9, 2025.
Pharma
Eli Lilly CEO Took Home $114 Million in 2024 Amid Record Profits and Perks: Eli Lilly CEO Dave Ricks made $114 million last year, a rare nine-figure payout for a health care executive, according to a new proxy statement. The company also reimbursed Ricks and two other executives for $186,000 in expenses related to a “global executive leadership meeting” held in Paris alongside the 2024 Olympics. Lilly’s soaring profits—$10.6 billion in 2024, more than double the previous year—were driven by its blockbuster GLP-1 drugs, Mounjaro and Zepbound. With investor enthusiasm for next-generation treatments, Lilly has become the world’s wealthiest health care company. “Lilly CEO Got a Big Payday (and an Olympics Treat),” STAT, March 12, 2025.
Pharmaceutical Companies Have Already Raised Prices on Over 800 Drugs in 2025: Drugmakers have increased the prices of more than 800 brand-name prescription drugs this year, with a median hike of 4%. Leadiant Pharmaceuticals raised prices significantly: by 15% to $149 per pill for Matulane, a Hodgkin disease treatment, and by 20% (to $2,597) for Cystaran, eye drops for cystinosis. The total number of price hikes has risen sharply from 140 announced in late December, with more expected by the end of 2025. “Big Pharma Has Already Raised the Prices of Hundreds of Drugs This Year,” Quartz, January 28, 2025.
Nearly 72 Million Americans Skipped Needed Care Due to Cost in 2024: The West Health-Gallup 2024 Survey on Aging in America found that an estimated 72.2 million adults—nearly one in three—did not seek necessary health care in the past three months (May-July 2024) due to cost, including 8.1 million Americans aged 65 and older. Additionally, nearly one-third (31%) of respondents expressed concern about affording prescription drugs in the next 12 months, a sharp rise from 25% in 2022. The findings highlight a worsening affordability crisis in the U.S. health care system. “Americans’ Ability to Afford Healthcare Hits New Low in 2024,” News Medical Life Sciences, July 17, 2024.
Majority of Congress Receives Significant Contributions from Pharmaceutical Industry: An analysis of OpenSecrets data found that most U.S. lawmakers receive substantial financial contributions from pharmaceutical and health product companies. On average, House Republicans received $45,000 and House Democrats $47,000, while Senate Republicans averaged $50,000 and Senate Democrats $69,000 in the 2024 election cycle. At least 72 of 100 U.S. senators received at least $10,000 from pharmaceutical PACs or employees, with 12 senators surpassing $100,000—including seven Democrats and five Republicans. The findings highlight the deep financial ties between lawmakers and the pharmaceutical industry. “How Many Members of Congress Receive Money from Pharmaceutical Company PACs?” DeseretNews, January 31, 2025.
Health Inequities
Medicare Advantage Networks Restrict Access to Racially Concordant Physicians: A Health Affairs report found that Medicare Advantage (MA) network limitations exacerbate racial and ethnic disparities by restricting access to Black and Hispanic physicians, who are known to improve preventive care use among these populations. Black and Hispanic physicians are underrepresented in MA networks compared to White physicians (43.2% and 44.0% vs. 51.1%), and many Black and Hispanic beneficiaries lack any in-network doctors of their race. In 41.3% of counties, there are no Black physicians in MA networks, while 47.2% of counties lack Hispanic physicians. These restrictions limit culturally competent care, reinforcing barriers to preventive services and worsening health disparities for MA enrollees. “Medicare Advantage Networks Include Few Black or Hispanic Physicians, Making Concordant Care Inaccessible for Many,” Health Affairs, January 2025.
MA Enrollees Report Widespread Unfair Treatment in Health Care: A Health Affairs study of 1,863 Medicare Advantage (MA) enrollees from 21 plans found that 9% reported experiencing unfair treatment in a health care setting, with the most common reasons being health condition (6%), disability (3%), and age (2%). Among those reporting unfair treatment, 40% cited multiple forms of discrimination. Enrollees qualifying for Medicare via disability were more likely to report unfair treatment based on disability, age, income, race and ethnicity, sex, sexual orientation, and gender identity. “Medicare Advantage Enrollees’ Reports of Unfair Treatment During Health Care Encounters,” Health Affairs, May 29, 2024.
Fewer High-Quality Medicare Advantage Plans Available in Socially Vulnerable Areas: A study found that markets with greater unmet social needs—measured by higher Social Vulnerability Index (SVI) scores—have fewer high-quality Medicare Advantage (MA) plans. The most vulnerable markets had 1.5 fewer MA plans overall and 1.1 fewer plans rated 4 stars or higher compared to the least vulnerable markets. This disparity was most pronounced in the southern U.S., where a higher proportion of Black/African American populations reside. “Association of Social Vulnerability and Access to Higher Quality Medicare Advantage Plans,” Journal of General Internal Medicine, December 20, 2024.
Medicare Advantage Enrollment Growth Among Racial Minorities Driven by Financial Barriers, Not Equity: While industry apologists point to the increasing enrollment of racial and ethnic minorities in Medicare Advantage (MA) as a sign of greater equity, research suggests this trend is largely driven by financial necessity rather than improved access to quality care. A study in The American Journal of Managed Care found that 40% of Black and Hispanic Medicare beneficiaries are near-poor, earning between 101% and 250% of the federal poverty level (FPL). These individuals do not qualify for Medicare supplemental insurance but often struggle to afford necessary care. Compared to White beneficiaries, Black and Hispanic enrollees are less likely to have savings or supplemental coverage, making MA’s lower cost-sharing and additional benefits an economic relief rather than a fundamental improvement in care access. “Racial/Ethnic Disparities in Cost-Related Barriers to Care Among Near-Poor Beneficiaries in Medicare Advantage vs Traditional Medicare,” The American Journal of Managed Care, October 23, 2024.
Medicare Advantage Attracts Low-Income Enrollees with Limited Benefits While Restricting Care: Claims that Medicare Advantage (MA) improves equity obscure the reality that many low-income beneficiaries choose these plans out of financial necessity rather than for superior care. A JAMA Health Forum study found that Black beneficiaries were 9.0 percentage points more likely to enroll in a plan with any dental benefit and 11.2 percentage points more likely to choose a comprehensive dental plan than White beneficiaries. However, this trend reflects cost-driven decision-making rather than expanded access to quality care. MA plans use zero-premium options and supplemental benefits to attract enrollees while simultaneously restricting provider networks and specialized care, ultimately reinforcing disparities rather than addressing them. “Enrollment Patterns of Medicare Advantage Beneficiaries by Dental, Vision, and Hearing Benefits,” JAMA Health Forum, January 12, 2024.
Burnout
Medicare Advantage Prior Authorization Delays Harm Patients, Fuel Burnout: A 2024 AMA survey found that over 90% of physicians, including those treating nursing home patients, reported that prior authorization (PA) delays have caused significant patient harm. For 24% of these doctors, the delays resulted in hospitalization, permanent disability, or death. Physicians spend an average of 12 hours per week handling 43 PA requests, contributing to widespread burnout; 95% cite PA as a reason for stress, and one in five are considering leaving medicine within two years. “‘Broken System’ of Medicare Advantage Prior Authorizations Leads to Nursing Home, Hospital Woes,” Skilled Nursing News, October 29, 2024.
Physician Burnout Continues to Drive Early Retirements and Exits in 2024: A MGMA Stat poll found that 27% of medical groups had a physician leave or retire early in 2024 due to burnout, while 41% reported that burnout worsened this year. Meanwhile, 45% said burnout levels remained the same as last year. The poll, based on 449 responses, highlights the persistent impact of burnout on the health care workforce, even as unexpected turnover stabilizes. “Physician Burnout Still a Major Factor Even as Unexpected Turnover Eases,” MGMA, September 4, 2024.
Higher Nurse Turnover Intentions Linked to Increased Patient Mortality: A multinational study analyzing data from 1,046 nurses across 15 public hospitals in Italy found a direct correlation between nurse intentions to quit and patient mortality. The study focused on surgical patients aged 50 and older who had hospital stays of at least two days. Researchers found that for every 10% increase in nurses intending to leave their jobs, inpatient hospital mortality rose by 14%. “Study Links Nurse Intention to Quit with Patient Mortality,” Health Policy, March 16, 2024.
Emergency Medicine Tops List of Most Burned-Out Specialties in 2024: A Healthgrades survey of 9,226 physicians across 26 specialties found that emergency medicine had the highest burnout rate at 63%, followed by obstetrics/gynecology (53%), oncology (53%), and pediatrics (51%). 42% of physicians said they had been burned out for over two years, and 16% considered leaving medicine due to burnout. Key contributors included excessive bureaucratic tasks, long work hours, lack of respect from colleagues, and inadequate compensation. “2024’s Most and Least Burned Out Physicians by Specialty,” Healthgrades, April 16, 2024.
Nearly Half of Physicians Report Burnout, While Depression Rates Remain Stagnant: A Medscape survey found that 47% of physicians are currently experiencing burnout, while 24% report depression—a rate that has remained unchanged since 2020. The findings reveal ongoing challenges in physician mental health, underscoring the need for workplace reforms and support systems. “‘If Boundaries Are Set, It Is Possible’: Medscape Physician Mental Health & Well-Being Report 2025,” Medscape, January 31, 2025.
Corporate Health Insurance
Humana Faces Billions in Losses After Medicare Advantage Ratings Drop: Humana, one of the largest Medicare Advantage providers, saw its stock plunge to a 15-year low after the federal government downgraded the rating for one of its major plans. In a filing to the SEC, Humana disclosed that only 1.6 million members—about 25% of its total—will be enrolled in Medicare Advantage plans rated four stars or higher in 2025, a sharp drop from 94% this year. CMS assigns star ratings based on factors like provider performance and plan administration, with higher ratings leading to lucrative government bonuses. A key Humana plan covering 45% of its Medicare Advantage members is expected to drop from 4.5 to 3.5 stars, potentially costing the company nearly $3 billion in 2026 bonus payments. Humana is appealing the rating but acknowledged its impact on future earnings. “Medicare Advantage Giant Humana Reels After Ratings Cut,” The Washington Post, October 2 2024.
UnitedHealth Faces Stock Decline Amid Medicare Billing Investigation and Industry Scrutiny: UnitedHealth’s Medicare Advantage division, the largest in the country with over 7.8 million enrollees, is under investigation by the U.S. Department of Justice for potential civil fraud related to its Medicare billing practices. When this story broke, it sent UnitedHealth’s stock plummeting more than 10% in pre-market trading, dropping over $52 to below $447 per share. Other Medicare Advantage insurers, including Humana, also saw stock declines. The company has faced mounting challenges, including increased health care usage, rate cuts, and a difficult period following the December shooting death of CEO Brian Thompson, which led to a sharp $100 drop in stock value. “UnitedHealth Stock Plummets Following US Medicare Billing Investigation Report,” CloudBrain, February 21, 2025.
Dr. Oz Tapped to Lead Medicare Despite Millions in Health Care Investments: President Trump’s pick to oversee the Centers for Medicare and Medicaid Services (CMS), Dr. Mehmet Oz, has reported owning up to $600,000 in stock from companies benefiting from private Medicare contracts. In 2022, Oz and his wife held at least $8.5 million in health care investments, including up to $550,000 in UnitedHealth Group stock and as much as $50,000 in CVS Health shares—both major Medicare Advantage insurers. As a Senate candidate, Oz promoted a “Medicare Advantage for All” plan, which would expand the privately run Medicare option despite research showing it costs taxpayers 22% more than traditional Medicare. “Dr. Oz is Trump’s Pick to Oversee Medicare. He Owns Healthcare Stocks That Could Benefit,” Quartz, November 20, 2024.
UnitedHealth Pushed Doctors to Inflate Diagnoses for Medicare Advantage Payments: Internal documents obtained by STAT News reveal that UnitedHealth pressured its physicians to add lucrative diagnoses to Medicare Advantage patients, boosting the company’s risk-adjusted payments by billions. A doctor leaderboard and $10,000 bonuses incentivized coding strategies that sometimes included clinically insignificant, marginally treatable, or even nonexistent conditions. The investigation exposes how UnitedHealth manipulated the payment system to maximize profits at Medicare’s expense. “Inside UnitedHealth’s Strategy to Pressure Physicians: $10,000 Bonuses and a Doctor Leaderboard,” STAT News, October 16, 2024.
PNHP Chapter Reports
Arizona
The Arizona chapter held two legislative meetings with staff from Sen. Gallego and Rep. Ciscomani’s offices to discuss Medicaid cuts, Medicare Advantage, threats to the ACA, and global issues such as reductions to U.S. aid. Medicare Advantage was a central focus in both discussions. Chapter leaders have also been encouraging members to complete the moral injury survey.
To get involved in Arizona, contact Dr. Eve Shapiro at shapiroe@u.arizona.edu.
California
The Bay Area chapter has remained connected through ongoing monthly meetings, where members have engaged in discussions on health care issues, including the mental health crisis and the harms of privatization. One notable highlight was the publication of “My Brother’s Keeper: The Untold Stories Behind the Business of Mental Health—and How to Stop the Abandonment of the Mentally Ill” by psychiatrist Nick Rosenlicht in October, which sparked thoughtful conversation within the group.
To get involved in the Bay Area, contact Dr. Henry Abrons at habrons@gmail.com.
The Humboldt County chapter has been highly active throughout the year, engaging in local, state, and national advocacy. Highlights include hosting Assembly candidate Chris Rogers at a chapter meeting, launching a “stealth advocacy” program to counter local Medicare Advantage promotion, and raising significant funds at the North Country Fair booth. Members also participated in Pastels on the Plaza to promote single payer and engaged in media outreach through ads, op-eds, and radio interviews. Chapter leaders attended the PNHP Annual Meeting in Chicago, contributed to the Office of Health Care Affordability (OCHA) educational forum, and are working closely with the Movement to End the Privatization of Medicare. The chapter also endorsed the National Single Payer Day of Action on May 15 and remains deeply involved in advocacy against Medicare privatization.
To get involved in Humboldt County, contact Dr. Corinne Frugoni or Patty Harvey at healthcareforallhumboldt@gmail.com.
The Los Angeles chapter initially held hybrid monthly meetings at the Santa Monica Library, but due to low attendance, they have transitioned to more accessible Zoom meetings on the fourth Saturday morning of each month. These gatherings feature lectures and discussions on key health care topics, offering members a space to stay informed and engaged.
To get involved in Los Angeles, contact Dr. Nancy Niparko, nniparko@gmail.com, or Dr. Maleah Grover, mgm1payer@gmail.com.
A chapter member in Santa Barbara recently participated in a delegation to Cuba to observe their healthc are system and later presented a health policy seminar to share key takeaways. The chapter is also planning a legislative visit with their U.S. Representative on March 20 to discuss the harms of Medicare Advantage and to encourage support for Rep. Jayapal’s letter to CMS. Additionally, on April 1, the chapter will visit a local high school with two pre-med students to discuss the importance of single-payer health care.
To get involved in Santa Barbara, contact Dr. Nancy Greep at ncgreep@gmail.com.
Colorado
On February 27, the Colorado chapter hosted a powerful webinar titled “Denied,” featuring real-life experiences from U.S. and Canadian doctors and medical office staff. The panel highlighted the stark contrast between the two health care systems, particularly the ease of access and administration in Canada. The chapter continues to hold monthly joint meetings with PNHP members and Medical Professionals for Universal Healthcare, fostering collaboration and strategy-sharing. Recent recruitment efforts have resulted in 40 members signing up with expiration dates in 2026. Advocacy efforts have included outreach to four congressional offices, including Reps. Jeff Hurd and Jason Crow. The chapter also contacted Sens. Michael Bennet and John Hickenlooper, urging them to vote against the nominations of RFK Jr. and Dr. Mehmet Oz, and reached out to Rep. Diana DeGette to ask her to oppose Dr. Oz and support Rep. Jayapal’s letter to rein in Medicare Advantage overpayments and deceptive recruitment tactics.
To get involved in Colorado, contact Dr. Leslie Reitman at Les.reitman@gmail.com.
Georgia

Georgia members met with the staff of Sens. Ossoff and Warnock, as well as Reps. Nikema Williams, Barry Loudermilk, and Rick Allen, to discuss the harms of Medicare Advantage and to encourage support for the Rep. Jayapal and Sen. Warren letters to CMS. Participants in these meetings included a large and engaged group of physicians, students, and advocates. On January 20, an op-ed by Dr. Belinda McIntosh and Dr. Toby Terwilliger was published in the Atlanta Journal-Constitution, raising awareness about the urgent need for a single-payer system. The chapter also co-hosted a candlelight vigil for the uninsured on February 16, featuring speakers and community members calling for universal health care. To support the Moral Injury campaign, the chapter hosted a one-hour training session focused on distributing the national survey to gather stories and data from health care workers.
To get involved in Georgia, contact Dr. Toby Terwilliger at toby.terwilliger@gmail.com.
Illinois

Illinois chapter leaders Dr. Sydney Doe and Dr. Winnie Lin participated in Second City’s “Funny You Should Care” event to raise funds and share PNHP’s key talking points through comedy and performance. Dr. Doe also gave a talk on Medicare Advantage and the case for single payer at the Ethical Humanist Society in Skokie. Additionally, Dr. Monica Maalouf and Dr. Claudia Fegan took part in a virtual forum hosted by the Health & Medicine Policy Research Group on February 13. The chapter has also organized several legislative meetings to encourage support for Rep. Jayapal’s letter to CMS. On February 19, members met with Rep. Jan Schakowsky (represented by Drs. Peter Gann, Deborah Geismar, and Anna Fogel) and with Rep. Sean Casten’s staff (attended by Drs. Ameer Sharifzadeh and Peter Gann). On February 25, Colin Garon and Dr. Peter Orris met with Rep. Mike Quigley’s staff.
To get involved in Illinois, contact Dr. Sydney Doe at sydney.doe94@gmail.com.
Kentucky
Members in Kentucky have been active in both community outreach and media. They tabled at World Fest and the Pride Festival, distributing flyers and gathering petition signatures to promote Enhanced Medicare for All. Kentuckians for Single-Payer Health Care also helped reorganize the SNaHP chapter at the University of Louisville in February. Additionally, they regularly produce Single Payer Radio, covering topics such as reproductive rights, the dangers of Medicare Advantage, and broader issues in the U.S. health care system. PNHP information on Medicare Advantage is featured at events and on the radio.
To get involved in Kentucky, contact Kay Tillow at nursenpo@aol.com.
Maine
Maine members have been active on both the federal and state levels. Between January 29 and February 5, Maine AllCare board members and supporters met with staff from Sens. Angus King and Susan Collins, and Rep. Jared Golden, to express concerns about MA—specifically, its overpayments and the impact on patient care. They also urged each office to support Rep. Jayapal’s letter calling for reforms to the MA program. On the state level, Maine AllCare is supporting three state bills: a universal health care study bill, the creation of an All Maine Health Program, and a moratorium on private equity and REIT ownership of hospitals. In addition, Maine AllCare has launched an LTE team, resulting in over a dozen letters and op-eds published across major state newspapers in the past six months, advancing the message of publicly-funded universal health care.
To get involved in Maine, contact Dr. Henk Goorhuis at info@maineallcare.org.
North Carolina
The North Carolina chapter hosted their 30th Anniversary Annual Meeting on October 6, 2024, featuring Rose Roach as keynote speaker and a presentation by Dr. Diljeet Singh via Zoom. The chapter launched a new initiative, Action Hours, including one on February 4, 2025, to oppose the nomination of RFK Jr. as HHS Secretary, and another on March 10, 2025, focused on preventing cuts to Medicaid. Two chapter members were nationally recognized for their advocacy work: Rebecca Cerese received the Health Justice Advocate of the Year Award from Families USA and Dr. Eleanor Greene received the Founder’s Award for Excellence in Advocacy, presented by Dr. Vivek Murthy on behalf of Doctors for America at their National Leadership Conference in June 2024. The chapter also actively participated in PNHP webinars and has been engaged in educating colleagues and fellow advocates about the harms of Medicare Advantage and the need for a single-payer system.
To get involved in North Carolina, contact Dr. Eleanor Greene at eleanorgreene@northstate.net, or Dr. Conny Morrison at conny.morrison@healthcareforallnc.org.
Ohio
The Cincinnati chapter recruited five new members, including four physicians and one nurse, bringing their chapter roster from 15 to 20 members. Three members gave a combined 15 presentations on single-payer health care reform to audiences of physicians, nursing students, and community groups. In autumn, the chapter launched a petition drive urging Rep. Greg Landsman to support the Congressional Progressive Caucus’s efforts to reform Medicare Advantage. The campaign collected over 500 signatures, which were scheduled to be delivered to Rep. Landsman in person, and which most likely inspired him to sign Rep. Jayapal’s MA letter in March. The chapter has maintained an ongoing dialogue with Rep. Landsman and his health policy aide, providing research and articles on profiteering by MA insurers.
To get involved in Cincinnati, contact Dr. Philip K. Lichtenstein at lichtensteinphil1@gmail.com.
Virginia

The Virginia chapter has been active on multiple fronts. Members, especially Dr. Bruce Silverman and Sandra Klassen, worked with state legislators on a bill that would allow Medicare Advantage enrollees to switch to traditional Medicare without underwriting—an effort that was unsuccessful this session, but will be pursued again. The chapter also formed a coalition with Arlington Medicare for All and the Northern Virginia DSA to advocate for Medicare for All and oppose Medicare Advantage. Raymond Uymatiao, MS4, helped launch a new SNaHP chapter at Virginia Tech Carilion and spoke at the People’s Action protest at UnitedHealthcare in D.C. Additionally, fourth year medical student Rachel Fox spoke at a Popular Democracy-led rally that included both Rep. Jayapal and Sen. Sanders as speakers. She focused on fighting Medicaid cuts and MA overpayments.
To get involved in Virginia, contact Dr. Robert Devereaux at robdev56@icloud.com.
Washington

The Washington state chapter has been deeply engaged in coalition building and education. They serve on the Steering Committee of Health Care is a Human Right Washington and co-organized the first-ever Single-Payer Summit, bringing together representatives from 20 organizations committed to single payer. The summit group continues to meet regularly. The chapter also holds monthly meetings featuring speakers on timely health care issues and sent a delegation of 12 PNHPWA and SNaHP WA members to the PNHP Annual Meeting in Chicago.
To get involved in Washington, contact Dr. David McLanahan at mcltan@comcast.net.
SNaHP Chapter Reports
SNaHP Rising (Western University)
SNaHP Rising (Western University) is among one of the newest chapters, and officially became recognized as a part of SNaHP on February 19. Their first meeting recruited eight medical students and included a discussion on the core arguments for single payer and the failures of MA. They also discussed the AAFP’s potential resolution opposing MA and encouraged students to submit their own testimonies to support.
To get involved with SNaHP Rising, contact Zollie Daily at zollie.daily@westernu.edu.
Florida SNaHP

Florida SNaHP members met with the offices of Reps. Maxwell Frost, Sheila Cherfilus-McCormick, Jared Moskowitz, and Frederica Wilson to encourage them to sign on to Rep. Jayapal’s letter calling for reform of Medicare Advantage. The chapter also hosted a powerful Town Hall with Reps. Jayapal and Cherfilus-McCormick to raise awareness about the dangers of Medicare privatization. The event drew 140 attendees on Zoom, and over 80 participants took action by emailing their representatives to oppose Medicare “Advantage.” In addition, the chapter held a successful Health Policy Week, adding over 60 new M1 members to their listserv and launching new student chapters at the UF undergraduate campus, UCF College of Medicine, and USF Morsani College of Medicine.
To get involved in Florida, contact Pat Haley at patrickhaley59@gmail.com.
FSU (Florida State University)
FSU (Florida State University) SNaHP members supported a February 2025 Town Hall featuring Rep. Pramila Jayapal and mobilized students during Medicare Open Enrollment with a national activist call. The chapter also met with Rep. Sheila Cherfilus-McCormick and participated in a June 2024 Town Hall with key health care leaders. Their efforts continue to raise awareness about the harms of Medicare Advantage and promote patient-centered reform.
To get involved with FSU SNaHP, contact Davalda Bellot at dmb12d@fsu.edu.
Health Care for All (Chicago College of Osteopathic Medicine)
The Health Care for All (Chicago College of Osteopathic Medicine) chapter hosted a screening and discussion of “The Healthcare Divide” to raise awareness about the disparities caused by our current health care system. They also organized a workshop on letter-writing campaigns, equipping participants with tools to effectively advocate for health care reform. Several members were actively involved in drafting and supporting resolutions related to Medicare Advantage, which were submitted to both the Illinois State Medical Society (ISMS) and the American Osteopathic Association (AOA).
To get involved with Health Care for All, contact Brittany Taylor at brittany.taylor1@midwestern.edu.
Northwestern SNaHP
In October 2024, Northwestern SNaHP students Samiya Manocha (M1) and Mo Kissinger (M4) collaborated with peers from other Illinois medical schools to write and submit a resolution to the Illinois State Medical Society (ISMS) urging greater transparency in Medicare Advantage plans. The resolution was recommended for adoption by committee and is set to be voted on in late April. From September to December 2024, students Emma Pauer and Laith Kayat (M2s) led a chapter book club on “Medicare for All: A Citizen’s Guide,” bringing members together for three in-depth discussions. The chapter also hosted a special event in December 2024, “A Conversation with Dr. Claudia Fegan,” where Dr. Fegan spoke to a large student audience about Medicare for All and international health care systems, sparking strong interest and dialogue.
To get involved at Northwestern, contact Becca Marcus at Rebecca.marcus@northwestern.edu.
University of Illinois College of Medicine – Peoria
The SNaHP chapter at the University of Illinois College of Medicine – Peoria held its first ever chapter meeting with an introductory lunch to kick off organizing efforts and build member engagement. Chapter leaders also attended the SNaHP conference, connecting with other medical students and advocates from across the country. In collaboration with UI Health residents and the Chicago PNHP chapter, the group began an investigation into billing practices at UI Health, aligning with broader efforts to uncover and address harmful health care system practices. They also shared the Moral Injury Survey with faculty to encourage participation and awareness.
To get involved in the Peoria chapter, contact Kelley Baumann at kbauma22@uic.edu.
Iowa SNaHP
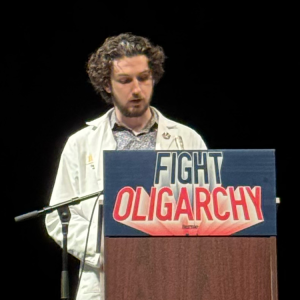
The Iowa SNaHP chapter launched in fall 2024 and has quickly gained momentum. From having no formal structure in September, the group now has around 40 members on paper, with 17 actively involved in planning and executing events. Their programming is widely advertised to the entire College of Medicine MD and PA student body. The chapter’s first event, “Single Payer 101” with Dr. Arya Zandvakili, took place on October 24, 2024, followed by a student-led presentation on Medicare DISadvantage on December 4, 2024, which utilized Dr. Ed Weisbart’s “Naked Profiteering” slide deck to highlight the advantages of traditional Medicare over Medicare Advantage. Most recently, I-SNaHP members attended the Sen. Bernie Sanders rally in Iowa City on February 22, 2025, where Zach Grissom was one of the speakers who addressed the crowd before the Senator, speaking about MA and Medicaid work requirements.
To get involved with I-SNaHP, contact Zach Grissom at zach-grissom@uiowa.edu.
KYCOM (University of Pikeville – Kentucky College of Osteopathic Medicine)
In partnership with Midwestern University Chicago College of Osteopathic Medicine, the KYCOM (University of Pikeville – Kentucky College of Osteopathic Medicine) SNaHP chapter submitted a SOMA resolution on the harmful effects of MA. Serina Sajjad, Adam Sayler, and Sammy Jaber were key contributors to the resolution’s writing and editing. The chapter also implemented a Community Aid initiative within the school’s student-run free clinic, launching the Bear Cove, a mutual aid corner offering food, hygiene products, clothing, and reproductive health supplies. The initiative, led by Cassie Craig and in partnership with All Access EKY, includes ongoing donation drives, needs assessments, and plans to expand into harm reduction services like Narcan training and safe needle disposal. In February, the chapter launched a statewide medical debt relief campaign in collaboration with Undue Medical Debt, aiming to abolish $33 million in defaulted medical debt across Kentucky. They also hosted an on-campus presentation highlighting how MA’s practices limit care and increase corporate profit. This training supported their Medicare Advantage Bingo events at Myers Tower and Pikeville Nursing and Rehabilitation Center, where students educated residents using interactive games, word searches, and coloring sheets. The events were led by Sammy Jaber and Serina Sajjad and co-hosted with the KYCOM Geriatrics Club.
To get involved with KYCOM SNaHP, contact Evan Hawthorn at EvanHawthorn@upike.edu.
WMed SNaHP

WMed SNaHP members launched their organizing efforts with a successful kickoff meeting on November 21, 2024. Chapter leadership presented on diabetes as a case for single payer health care to an audience of over 30 peers and gathered signatures for MI for Single Payer’s petition supporting the MICARE initiative for state-based Medicare for All. The chapter has also formed partnerships with Southwest Michigan DSA and Food Not Bombs, collaborating on two ongoing projects to serve the local community directly. In addition, chapter leaders attended the SNaHP Medicare Advantage meeting and have been distributing PNHP materials on Medicare Advantage to raise awareness among peers.
To get involved with the WMU Homer Stryker chapter, contact Genevieve Nicolow at genevieve.nicolow@wmed.edu.
Creighton SNaHP
The Creighton SNaHP chapter hosted two successful Undue Medical Debt fundraisers—Dance Off Debt on October 4 and a Bake Sale on January 27—raising over $8,500 to help eliminate medical debt. On the legislative front, members testified in support of a Nebraska state bill to strengthen protections against medical debt garnishment on January 24. Additionally, the chapter held meetings with the offices of Sen. Deb Fischer (2/11) and Rep. Don Bacon (2/12) to advocate for strengthening traditional Medicare and opposing Medicare Advantage rate hikes. The chapter also created and delivered an educational presentation, “How to Navigate the U.S. Health Care System,” for a local community organization. Accompanied by a handout and map translated into 13 languages, these materials were distributed at a local health fair and will soon be available on the chapter’s website to expand access even further.
To get involved with the Creighton chapter, contact Luci Lange at lkl94259@creighton.edu.
Jacobs SNaHP
In October, the Jacobs SNaHP chapter hosted a fun and educational SNaHP Trivia Night, with questions focused on single-payer health care. The event was held at a local bar and featured prizes for the top three teams, helping to engage students in a relaxed and informative setting. In addition to campus activities, the chapter has been collaborating with other SNaHP chapters across Western New York, meeting monthly to strategize on lobbying local politicians in support of health care justice and Medicare for All.
To get involved with the Jacobs SNaHP chapter, contact Dylan Wong at dkwong2@buffalo.edu or jacobssnahp@gmail.com.
SNaHP at NEOMED (Northeast Ohio Medical University)
In February, SNaHP at NEOMED (Northeast Ohio Medical University) board members Elsa Khan and Shannon Lam led a workshop as part of a required clinical skills and ethics course. Shannon Lam and Noyonikaa Gupta also published an op-ed in The Portager addressing concerns about proposed work requirements for Medicaid and Medicare. Members Helen Aziz and Shannon Lam also volunteered at the Teddy Bear Clinic to connect with children, helping foster an early interest in medicine and ease anxieties about visiting the doctor.
To get involved with the NEOMED SNaHP chapter, contact Shannon Lam at slam2@neomed.edu.
DUCOM (Drexel University College of Medicine)
In August, the DUCOM (Drexel University College of Medicine) SNaHP chapter hosted a Single Payer 101 event to introduce incoming M1s to the concept of single-payer health care and the mission of SNaHP. Later in the year, former board member Justin Yeung organized a hybrid talk with Dr. Ed Weisbart, who presented on the dangers of Medicare Advantage followed by a Q&A session with medical students. In addition to educational events, the chapter also participated in voter registration canvassing during the summer and early fall, partnering with Penn Medicine to reach community members and promote civic engagement.
To get involved with DUCOM SNaHP, contact Kacie Wheeler at ducom.snahp@gmail.com.
SKMC (Sidney Kimmel Medical College)
This year, the SKMC (Sidney Kimmel Medical College) SNaHP chapter hosted several informative speaker events, including a session with Dr. Julie Qualtieri focused on Medicare Advantage and a visit from Dr. Joe Jarvis of Utah, who shared insights from the Utah Cares campaign and offered strategic lessons for Pennsylvania. Looking ahead, the chapter plans to increase event attendance and visibility on campus, beginning with an upcoming student-run workshop on the Affordable Care Act and threats to its subsidies under the Inflation Reduction Act. The chapter plans to continue outreach to local elected officials to promote single-payer policies and highlight the growing support among health care worker unions. In the policy space, the chapter is building connections with other student organizations at Jefferson. They are currently working with the Jefferson AMA chapter to organize a policy-writing workshop, with the goal of submitting single-payer focused resolutions to PAMED.
To get involved with the SKMC chapter, contact Emily Hashem at enh013@students.jefferson.edu.
Responding to the UnitedHealthcare CEO Murder
Four months ago, the shocking news broke that the CEO of UnitedHealthcare had been shot and killed in Manhattan while on his way to the company’s annual investor conference. Public reaction to this event has been intense, sparking a national conversation about corporate control of health care and the deep frustration felt by Americans towards private insurance companies. This moment underscored a stark reality: Our health care system is in crisis, and people are suffering under the weight of corporate greed.
PNHP has been vocal in responding to this event, with our members highlighting the urgent need for Medicare for All as the only solution to the injustices perpetrated by private insurers. PNHP National Coordinator Dr. Claudia Fegan published a powerful op-ed in Common Dreams in early January, reflecting on her decades of difficult experiences, and how these are shared by millions of Americans who struggle to receive the care they need.
“I have seen patients suffer and die in order to pad the bottom lines of corporate health insurers,” she wrote, “and in recent years I have seen this problem getting much worse. These are the stories that Americans are sharing in this fraught moment. We have to ask ourselves: Are we listening? And what are we going to do about it?”
The public reaction to this shooting has made one thing clear: Americans are fed up with private insurers profiting off of denied care, surprise bills, and administrative hurdles that make it harder for patients to get the treatment they need. As this story dominated the news cycle, PNHP leaders and members took the opportunity to shift the conversation toward real solutions—not just outrage, but action. Our members have been speaking out in the media, engaging in public discussions, and emphasizing that the only way to truly end the suffering caused by corporate insurers is to replace them with a single-payer Medicare for All system.
This moment is a wake-up call, and we cannot afford to ignore it. PNHP will continue to fight for a health care system that puts patients before profits, and we urge our members and supporters to channel their frustration into advocacy.
PNHP in the News
News items featuring PNHP members
- “North Carolina hospital company forgives debts of 11,500 people after NBC News report,” NBC, 9/20/2024
- “Doctors ‘fight like hell’ against a second Trump admin: ‘Elections do matter for your health,’” Politico, 9/21/2024
- “Is public, quality healthcare possible in the United States?,” People’s Dispatch, 12/17/2024
- “CEO murder exposes growing anger with the corporate health system,” KALW, 12/17/2024
- “Insurance CEO Murder Exposes Deep Anger at US For-Profit Healthcare,” BTL Online, 12/16/2024
- “Mother Jones Daily,” Mother Jones, 12/16/2024
Op-eds by PNHP members
- “Jennifer Coffey: It’s not Medicare and it’s no advantage,” Union Leader, 12/24/2024
- “Dr James Fieseher: Medicare Advantage Plans are the Junk Bonds of Healthcare,” Union Leader, 12/30/2024
- “Another Voice: Medicare Open Enrollment Period Still Bed Eviling,” Buffalo News, 11/2/2024
- “The Trouble With Upcoding Extends Far Beyond Ethics,” MedPage Today, 11/11/2024
- “Our health care system includes a lot of hidden costs,” Bangor Daily News, 11/12/2024
- “A Daughter’s Fight to Protect Her Parents from Costly Pitfalls of Medicare Advantage,” HEALTH CARE un-covered, 11/13/2024
- “Column: Health care policy hurts Hawaii patients,” The Honolulu Star-Advertiser, 9/25/2024
- “The Humana Wall Street/Medicare Advantage Love Story Seems to Be Ending,” HEALTH CARE un-covered, 10/4/2024
- “OPINION: ‘Dismissed!’,” Advance, 1/3/2025
- “Health care in U.S. must be better,” The Baltimore Sun, 12/27/2024
- “Yes, condemn CEO’s murder, but know why people feel rage toward health insurers,” The Tennessean, 12/16/2024
- “If you reflexively blamed this insurer for its proposed anesthesia policy, you were right,” MSNBC, 12/11/2024
- “Americans Are Angry About Their Health Insurance—With Good Reason,” Common Dreams”, 1/1/2025
- “I Was a Health Insurance Executive. What I Saw Made Me Quit.,” The New York Times, 12/18/2024
- “Don’t Make This Mistake During Open Enrollment,” MSN, 11/21/2024
Letters to the editor by PNHP members
- “Readers sound off on Medicare Advantage’s business model, banned books week and medication abortions,” New York Daily News, 9/21/2024
- “Project 2025 would hurt Mainers,” Ellsworth American, 9/13/2024
- “Letter: It’s time to demand a better health care system,” Portland Press Herald, 10/05/2024
- “Medicare Insurers to Get Billions in Extra Payments,” Wall Street Journal, 10/24/2024
- “Medicare Advantage is no advantage to patients,” Atlanta Journal-Constitution, 10/28/2024
- “Hurricanes, Climate Change and the Election,” New York Times, 10/11/2024
- “Commentary: More than ever, we need the New York Health Act,” Times Union, 12/13/2024
- “Readers Write: Government efficiency, Abundant Life shooting, Time’s Person of the Year,” Star Tribune, 12/18/2024
- “Letter: Remove profits from patient care,” Bangor Daily News, 12/13/2024
- “Letter: Op-ed was right about health care,” Portland Press Herald, 12/27/2024
- “The despair behind the sarcastic response to an insurance CEO’s killing,” Washington Post, 12/11/2024
- “Letters: If California’s fight against Trump becomes a losing cause, here’s what the state should do,” San Francisco Chronicle, 12/9/2024
- “America’s unjust health system finally gets a hard look after insurance CEO’s killing,” Los Angeles Times, 12/10/2024
- “Ways to Fix the Health Insurance Debacle,” New York Times, 12/16/2024
- “With apologies to World War II vets,” Chattanooga Times Free Press, 11/16/2024
- “Letters: The real threat to health care is not doctors,” Chicago Tribune, 12/31/2024
- “Money in Politics, Healthcare Top Nation’s Worries,” The Advance, 3/3/2025
- “Letter: RFK Jr.’s appointment is a disgrace,” Portland Press Herald, 02/28/2024