By Betty Keller, M.D.
The Barre-Montpelier (Vt.) Times Argus, Letters, Aug. 27, 2025
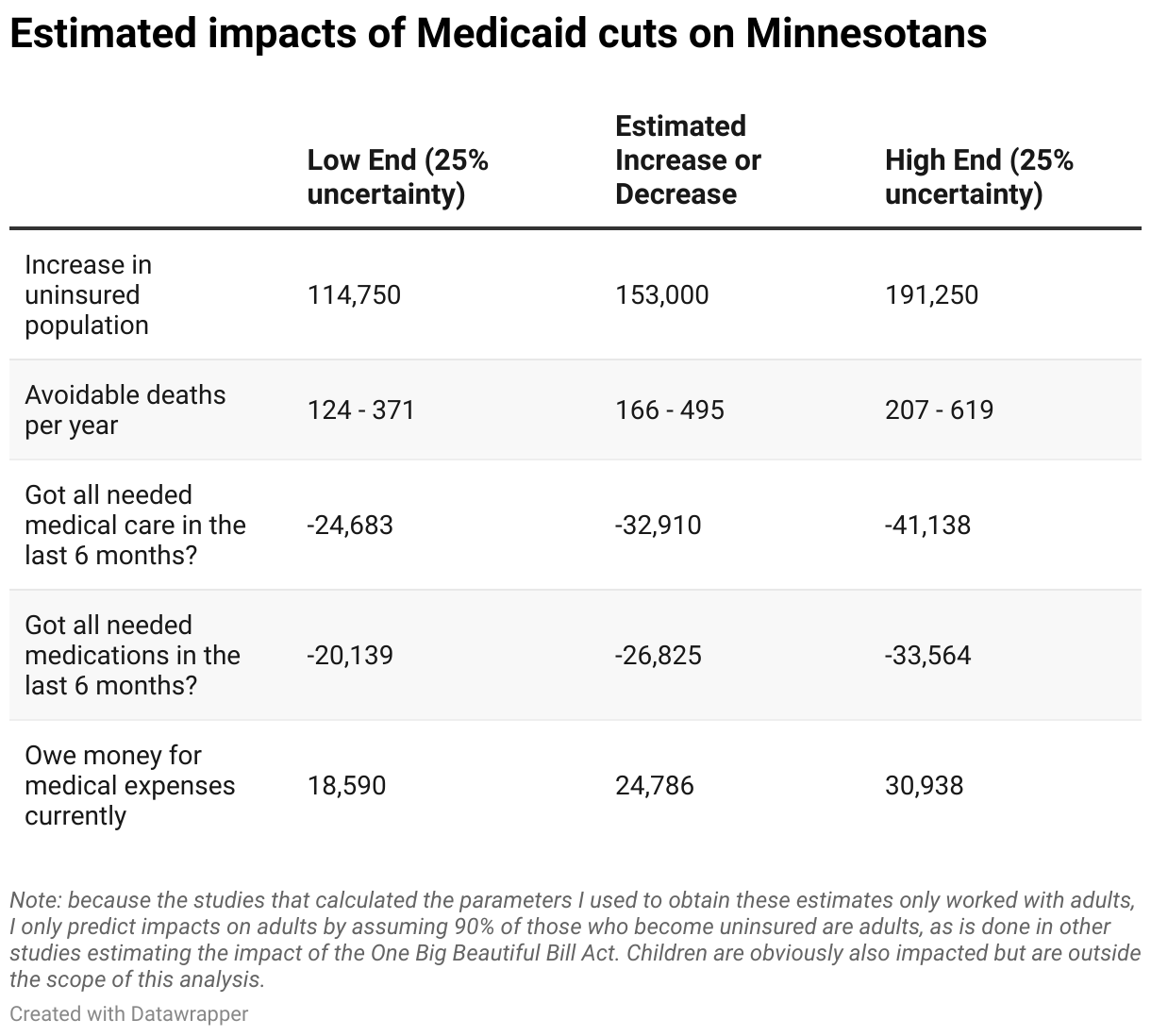
Medicaid pays for the health care of some 119,000 Vermonters. Vermont Agency of Human Services estimates 45,000 of them will end up uninsured as a result of the misnamed “One Big Beautiful Bill Act.” The impact on those people is obvious: avoiding doctor visits as long as possible, while their condition worsens, frequently resulting in emergency room visits, higher costs, worse outcomes, and even avoidable deaths.
The impact on the rest of us is less obvious. Think Medicaid has no impact on you if you aren’t on it? That’s a serious misconception. The $2.3 billion Medicaid feeds into Vermont’s health care system amounts to 27% of all health care spending in the state. Some 62% of that currently comes from the federal government. If that essential funding stops for 45,000 people, health care providers won’t get paid when all those now-uninsured people seek care. To compensate, most will likely raise prices for everyone else, including you. That’s not a sustainable solution.
These cuts will add serious strains to our already strained hospitals, which are already dropping services they deem unprofitable. What additional services will become unavailable, at which hospitals, affecting everyone, including people who do have insurance?
Did the people who concocted these new rules understand the consequences beyond those for the individuals losing coverage? Perhaps that is why they timed them to take effect after the midterm elections, so voters would be lulled into thinking all the naysayers were exaggerating or even making up the harms.
Please spread the word. Tell your friends and relatives, especially those in states where their elected officials voted for this huge disaster. Do what you can to push our elected officials to fix this.
Dr. Keller is president of Vermont Physicians for a National Health Program.