Wash your hands. Practice social distancing. And fight for a single-payer national health program that can address public health crises like the COVID-19 pandemic. Our fractured and inefficient collection of private and public health programs leaves millions of Americans out in the cold. A well-designed national health program would cover every U.S. resident and would ensure timely care for those who need it most.
Protecting public health during the immediate crisis
For the latest information on the COVID-19 pandemic, including recommended mitigation techniques, visit the Centers for Disease Control and Prevention website.
Read, sign, and share this important letter from the Committee to Protect Medicare demanding widespread COVID-19 testing, a national shelter-in-place order, and increased production of personal protective equipment.
For a continuously updated list of resources available to undocumented immigrants, see this Google Sheet compiled by the Betancourt Macias Family Scholarship Foundation.
For a continuously updated list of resources available to people with disabilities, see this dedicated webpage compiled by Access Living.
Coronavirus-related policy proposals and research
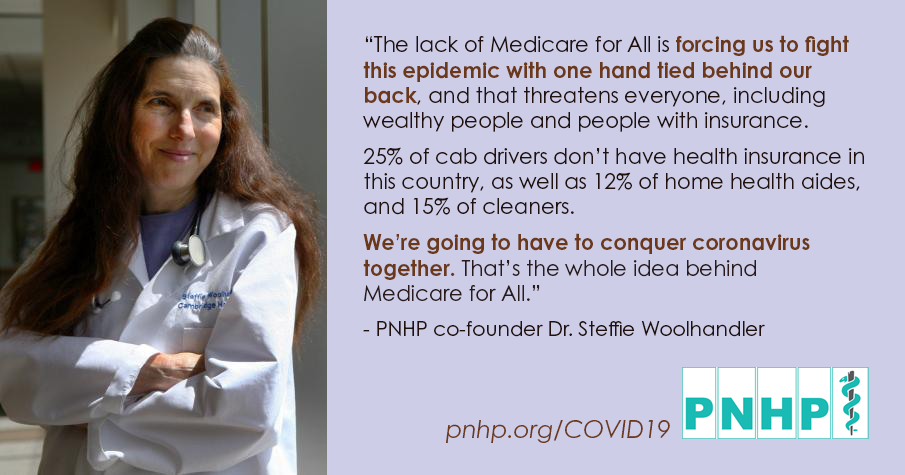
Physicians for a National Health Program has developed an eight-point plan of needed steps to fight COVID-19 including, but not limited to, single-payer Medicare for All. Our proposal was published in Boston Review, and can also be found at pnhp.org/COVID19Response.
PNHP leaders and allies have also published several studies detailing how job loss, chronic health conditions, mass incarceration, and other inequities put millions at risk of contracting, and dying from, COVID-19:
- “We Are All in This Together: COVID-19 and the Case for Medicare for All,” by Hebah Kassem, Congressional Progressive Caucus Center, March 2021.
- “Unprepared for COVID-19: How the Pandemic Makes the Case for Medicare for All,” by Eagan Kemp, Public Citizen, March 16, 2021. (Public Citizen press release here.)
- “Risk for Severe COVID-19 Illness Among Teachers and Adults Living With School-Aged Children,” by Adam W. Gaffney, M.D., M.P.H.; David U. Himmelstein, M.D.; and Steffie Woolhandler, M.D., M.P.H., Annals of Internal Medicine, August 21, 2020. (PNHP press release here.)
- “Illness-Related Work Absence in Mid-April Was Highest on Record,” by Adam W. Gaffney, M.D., M.P.H.; David U. Himmelstein, M.D.; and Steffie Woolhandler, M.D., M.P.H., JAMA Internal Medicine, published online July 27, 2020. (PNHP press release here.)
- “Feasibility of Separate Rooms for Home Isolation and Quarantine for COVID-19 in the United States,” by Ashwini R. Sehgal, M.D.; David U. Himmelstein, M.D.; and Steffie Woolhandler, M.D., M.P.H., Annals of Internal Medicine, published online July 21, 2020. (PNHP press release here.)
- “18.2 Million Individuals at Increased Risk of Severe COVID-19 Illness Are Un- or Underinsured,” by Adam W. Gaffney, M.D., M.P.H.; Laura Hawks, M.D.; David H. Bor, M.D.; Steffie Woolhandler, M.D., M.P.H.; David U. Himmelstein, M.D.; and Danny McCormick, M.D., Journal of General Internal Medicine, published online June 10, 2020. (PNHP press release here.)
- “COVID-19 and US Health Financing: Perils and Possibilities,” by Adam Gaffney, M.D., M.P.H.; David U. Himmelstein, M.D.; and Steffie Woolhandler, M.D., M.P.H., International Journal of Health Services, published online June 9, 2020. (Full study on the PNHP website here.)
- “Insurers’ Offers of Free Care for Coronavirus Are Often Confusing and Limited,” by Eagan Kemp, Melinda St. Louis, Taylor Lincoln, and Mike Tanglis, Public Citizen, May 7, 2020.
- “Health Insurance Status and Risk Factors for Poor Outcomes with COVID-19 Among U.S. Health Care Workers: A Cross-Sectional Study,” by David U. Himmelstein, M.D. and Steffie Woolhandler, M.D., M.P.H., Annals of Internal Medicine, April 28, 2020. (PNHP press release here.)
- “COVID-19 in Prisons and Jails in the United States,” by Laura Hawks, M.D.; Steffie Woolhandler, M.D., M.P.H.; and Danny McCormick, M.D., M.P.H., JAMA Internal Medicine, published online April 28, 2020. (PNHP press release here.)
- “Intersecting U.S. Epidemics: COVID-19 and Lack of Health Insurance,” by Steffie Woolhandler, M.D., M.P.H., F.A.C.P. and David U. Himmelstein, M.D., F.A.C.P., Annals of Internal Medicine, published online April 7, 2020. (PNHP press release here.)
In response to the current crisis, PNHP recommends enrolling all currently uninsured U.S. residents in traditional Medicare, a time-tested program that already covers tens of millions of Americans.
Why we need improved Medicare for All
Whatever public health measures we can put in place to address COVID-19 are sadly limited by the awful state of our health care financing apparatus, and by the threadbare nature of our social safety net.
Congress can have a positive immediate impact by passing protections for workers, creating medical “sanctuaries” for undocumented immigrants, and eliminating out-of-pocket expenses for patients undergoing testing and treatment for COVID-19. But the only permanent solution is to enact a single-payer national health program that would:
- Cover all U.S. residents for all medically necessary care;
- Totally eliminate out-of-pocket spending;
- Guarantee appropriate health resources in all communities based on medical need;
- Increase public health spending and invest in research to improve population health; and
- Maintain the capacity to respond to nationwide crises in a unified manner.
COVID-19 is just one dramatic example of our failure to care for vulnerable patients and marginalized populations. To the extent that Congress passes laudable reforms, those reforms should not be allowed to expire, but should act as a catalyst in our push for single-payer reform.
If a concerted focus on public health is required to address the current crisis, then it is also required to address the ongoing crisis.
Organizing during the COVID-19 pandemic
As large public gatherings are cancelled across the country, PNHP activists are no doubt wondering how to safely maintain their vital single-payer advocacy in the age of “social distancing.” Our organizing team has developed two important guides for members to continue their work remotely:
- “Digital Organizing Swaps: An action plan for activists during COVID-19” details digital alternatives to planned in-person activities such as chapter meetings and canvassing events.
- “How to run a large conference call” provides tips for members to help make upcoming conference calls a success, including steps to take before, during, and after your call.
- “Zoom tips and tricks” will help members make the most of the Zoom video conferencing platform. Developed by Shannon Rotolo, PharmD.
If you have questions about organizing amidst COVID-19, email our organizing team at organizer@pnhp.org.