The global COVID-19 pandemic has hit the United States especially hard, with the fractured and inequitable state of U.S. health care and a lack of urgency on the part of some policymakers making matters even worse. PNHP has developed an eight-point plan of steps needed to confront COVID-19, which was published April 3, 2020 in Boston Review, and is reproduced below.
Physicians for a National Health Program (PNHP) Statement
COVID-19 cases have been identified in all 50 US states, a surge of hospitalizations is underway in some cities, and more than 5000 had died of the illness by early April. Meanwhile, unprecedented public health measures undertaken to slow the spread of the outbreak look certain to provoke a recession, with job losses for millions or tens of millions of workers. The nation is facing this outbreak and the looming recession with a dangerously fragmented and privatized health system. At the start of the crisis, 30 million people were uninsured1 and 44 million more underinsured2; around one in three Americans went without needed medical care because of costs2; and medical bankruptcies were commonplace.3 These problems will worsen as the economy spirals downward and hospitalizations rise.
Since its founding in the late 1980s, Physicians for a National Health Program (PNHP) has called for a single-payer, expanded and improved “Medicare for All” reform to ensure that everyone in the nation has health insurance that would: eliminate cost barriers that keep our patients from needed care; improve health outcomes; and free physicians to focus on patient care, not wasteful billing and clerical activities that sap needed time and resources.4-6 The COVID-19 crisis intensifies the urgency of such reform. It also calls for additional measures to fully protect all of our patients, including the most disadvantaged. We present, below, recommendations for measures needed to minimize hardship and loss of life during the COVID-19 pandemic and its aftermath.
– Adam Gaffney, M.D., M.P.H., PNHP President
1. Immediately protect patients from medical costs due to COVID-19
Recently-passed legislation eliminated cost-sharing for COVID-19-related diagnostic testing, and provided coverage of testing for the uninsured. However, it did not expand coverage of treatment, leaving tens of millions of Americans at risk of financial disaster in the face of illness. Even those with insurance who are treated at an in-network hospital are likely to be stuck with thousands of dollars in copays and deductibles. For the uninsured (or the insured who are treated “out-of-network”), costs are likely to rise to tens, or even hundreds of thousands of dollars.7-9
PNHP calls on Congress and the President to immediately enact legislation providing full coverage for all COVID-19-related care for everyone in the United States. Such a measure would protect patients who are infected, and ensure that those with symptoms do not delay seeking testing and care.
2. Implement universal coverage through a Medicare-for-All reform
Covering the costs of COVID-19 related care is not enough. In the impending recession, millions will lose jobs, income and health insurance, exacerbating the healthcare cost crisis. Some, including those with severe COVID-19 infections, will require costly long-term care. Medicare for All reform would guarantee coverage for everyone in the United States; eliminate cost barriers for needed care, whether for COVID-19 or other conditions; and ensure that precious healthcare dollars are spent on care — not wasteful bureaucracy10, corporate profits, or unnecessary, but lucrative interventions. Such reform is needed now more than ever.
3. Restore our public health infrastructure
Public health agencies are our first line of defense against novel epidemics. However, chronic underfunding of our federal, state, and local public health agencies impeded the response to this outbreak, exemplified by the ongoing diagnostic testing fiasco.11,12 Funding cuts have forced state and local public health agencies to eliminate 50,000 positions, a 20% decrease in the frontline workforce for fighting epidemics.13 The shortfall in resources has led some local public health authorities to give up14 on the case identification and contact tracing efforts that other nations have successfully employed to control spread of the epidemic.15
PNHP calls for increased federal funding to raise the share of national health expenditures devoted to public health and prevention from 2.5% to 5.0%. Bolstering the public health infrastructure is vital to combat the current pandemic, and to address other public health needs.
4. Protect incarcerated patients
Our nation’s densely crowded jails and prisons, which house the largest incarcerated population in the world, put inmates, staff and communities at grave risk of COVID-19. Outbreaks are already being reported among this uniquely vulnerable population.16
In addition to guaranteed healthcare access for the incarcerated population, PNHP joins other groups in calling for measures to reduce the at-risk population: the release of persons in pretrial detention or incarcerated for technical violations of parole or probation; stopping arrests for low-level offenses; early release where possible, especially for persons at increased health risk due to advanced age (a group known to have a low risk of re-offending) or co-morbidities.17
Universal coverage via Medicare for All would also ensure that individuals have adequate healthcare access in their communities after release from incarceration.
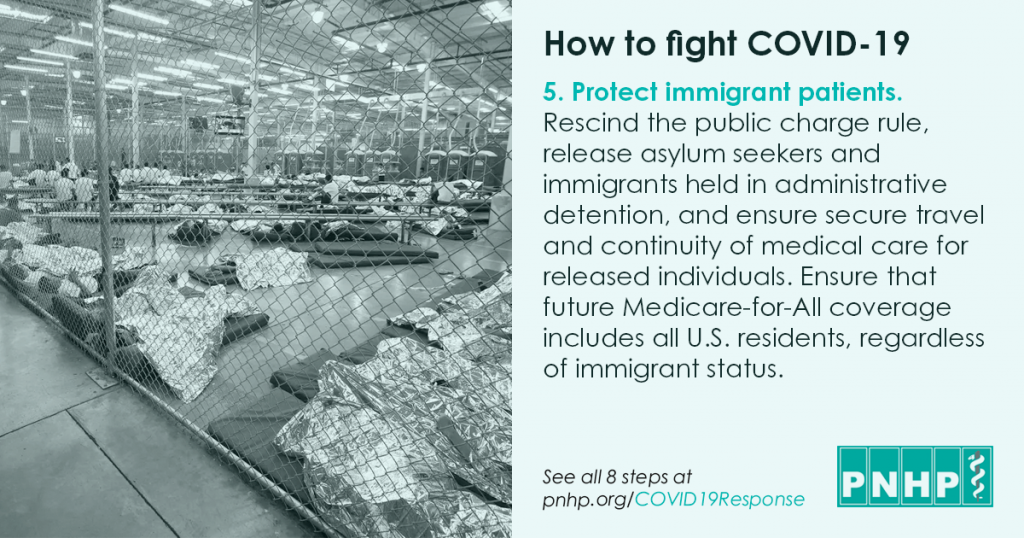
5. Protect immigrant patients
The Trump administration’s public charge rule, which imposes penalties on immigrant families for enrolling in social programs like Medicaid, will lead many to avoid needed testing or treatment for COVID-19,18 even though such care is technically exempt from the rule.19 Meanwhile, immigrants and asylum seekers in Immigration, Customs, and Enforcement (ICE) detention facilities are at serious risk from a COVID-19 outbreak; such facilities are crowded and are often in remote locations with limited accessibility to medical care.20
PNHP urges the federal government to rescind the public charge rule, and joins other human rights organizations in calling for ICE to release asylum seekers and immigrants held in administrative detention, and to ensure secure travel and continuity of medical care for released individuals.20 Additionally, PNHP calls for a universal Medicare-for-All coverage expansion to cover all US residents regardless of immigrant status.
6. Stabilize hospital financing while protecting patients from hospital costs
In the face of the coronavirus threat, hospitals across the country have cancelled elective procedures and stockpiled supplies, leading to falling revenue and rising costs.21 For some hospitals, particularly smaller rural hospitals, the coronavirus crisis could lead to closure.21 In response, recent legislation provided almost $100 billion in relief to the nation’s hospitals.22
Our nation can ill afford hospital closures, particularly at this moment. However, reform is also needed in how hospitals are paid to ensure their stability in the face of future crises, and to protect patients, who have faced lawsuits, wage garnishment, and home foreclosures as a result of hospital efforts to recoup medical debt.23 Hospital associations, meanwhile, continue to spend precious resources lobbying against public insurance expansions. PNHP hence calls for action from the nation’s community hospitals, the American Hospital Association, and the federal government.
Hospitals must end all lawsuits against patients for medical bills, including those hospitalized for COVID-19. The AHA should cease spending member hospitals’ funds on lobbying efforts against Medicare-for-All and other coverage expansions. In particular the AHA should withdraw from, and stop contributing to, the Partnership for America’s Healthcare Future, a dark-money lobbying group.
Finally, PNHP calls on the federal government to take action. It should replace hospitals’ current per-patient payment system with global budget funding similar to how fire departments are paid. This would free up substantial funds that hospitals currently spend on administration, which could be redirected to patient care — including for infectious disease-related surges.24 Global budgets would also ensure that hospitals are not dependent on lucrative elective procedures for their financial stability, and that hospitals caring for disproportionate numbers of poor and poorly-insured individuals have adequate resources. Finally, such a reform of hospital financing should include separate and dedicated funding for new hospital infrastructure, to ensure that an adequate and equitable supply of infrastructure — including hospital beds, ICUs, and a reserve supply of emergency equipment and protective gear — are available throughout the nation. Until then, the federal government should take direct action and provide necessary funding to procure needed personal protective equipment for the nation’s hospital workers.
7. Ensure that pharmaceuticals and vaccines — including for COVID-19 — are affordable for the public
A recent bill signed into law by President Trump provided needed funds for the development of drugs and vaccines for COVID-19. However, the new law will not ensure that patients could afford the newly-developed therapeutics.25
The current crisis underlines the need for the comprehensive pharmaceutical reform policy advocated by PNHP.26 We call for increased public drug R&D, including publicly-financed clinical trials. However, publicly-developed therapeutics — including for COVID-19 — should remain in the public domain, and be available to patients without charge. Additionally, prescription drug supply chains are threatened by the COVID-19 crisis, which could lead to shortages of essential medicines.27 The US should establish public drug manufacturing capacity as one backup to address such shortfalls.26
8. International considerations
Every nation faces major challenges fighting COVID-19. Some current US policies hinder other nations’ responses to the pandemic, and the global cooperation vital to containment. PNHP hence recommends easing or ending international sanctions that disrupt nations’ ability to respond to COVID-19. Additionally, the US should eliminate intellectual property constraints like patents and trade agreements that might restrict the low-cost production and distribution of essential drugs and vaccines, including those developed from publicly-funded research. Finally, we call for an end to the racist and xenophobic rhetoric that sows division and undermines cooperation.
The steps outlined above focus on public health and medical measures. With recession on the horizon, however, additional measures are needed to ameliorate impoverishment and social dislocation. Mass unemployment and economic privation will harm the nation’s health unless sweeping measures to strengthen the social safety-net are enacted. Such steps go beyond the scope of this document, but are critical for protecting the health and welfare of our patients.
There is much uncertainty in how severe the COVID-19 outbreak will ultimately prove to be in the United States. The rapid rise of cases and deaths, however, gives little reason for optimism. While no single policy could have prevented this outbreak, a robust, adequately-funded public health infrastructure and adherence to science-based policy — together with a universal publicly-funded national health program with unified financing and governance — would be powerful tools to control it. Change is sorely needed: to protect our patients during this pandemic, and other threats that will follow.
Addendum: Protect residents and staff of long-term care facilities
Note: This important step does not appear in the original Boston Review piece; it was developed by the Illinois Single-Payer Coalition Working Group on Long-Term Care and added to PNHP’s proposal in early 2021.
Residents of long-term care facilities, like residents of other congregate settings, have suffered disproportionate numbers of COVID-19 infections and deaths.28
Even before the pandemic, infection control, staffing ratios, and public health surveillance were inadequate, and injuries and deaths due to abuse and neglect were commonplace. All of these conditions have worsened during the pandemic.
Long-term care facility staff have also suffered illness and death.
Disability rights activists have fought for decades for the right to live in the community, with necessary services and supports, instead of in institutions.29 The pandemic proves the urgency of their demands.
PNHP’s 1991 proposal for a national long-term care program30 supported the demand for home and community-based services (HCBS), as has national improved Medicare for all legislation.
PNHP urges Congress to continue to include support for HCBS in the federal response to the pandemic; and urges the Centers for Medicare and Medicaid Services to issue guidance that explicitly enables local agencies to use appropriate HCBS funding for emergency relocation of residents of long-term care facilities and other congregate settings into safer housing, with needed supports.
Universal coverage of long-term care under Medicare for all would assure equitable funding of HCBS throughout the country.
References
- Cohen RA, Terlizzi EP, Martinez ME. Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, 2018 [Internet]. National Center for Health Statistics; 2019. [cited 2019 Aug 20]. Available from: https://www.cdc.gov…
- Collins SR, Bhupal HK, Doty MM. Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured [Internet]. Commonwealth Fund; 2019. [cited 2019 Nov 25]. Available from: https://www.commonwealthfund.org…
- Himmelstein DU, Lawless RM, Thorne D, Foohey P, Woolhandler S. Medical Bankruptcy: Still Common Despite the Affordable Care Act. Am J Public Health 2019;109(3):431–3.
- Himmelstein DU, Woolhandler S. A National Health Program for the United States. New England Journal of Medicine 1989;320(2):102–8.
- Gaffney A, Woolhandler S, Angell M, Himmelstein DU. Moving Forward From the Affordable Care Act to a Single-Payer System. Am J Public Health 2016;106(6):987–8.
- Woolhandler S, Himmelstein DU, Angell M, Young QD, Physicians’ Working Group for Single-Payer National Health Insurance. Proposal of the Physicians’ Working Group for Single-Payer National Health Insurance. JAMA: The Journal of the American Medical Association 2003;290(6):798–805.
- Potential costs of coronavirus treatment for people with employer coverage [Internet]. Peterson-Kaiser Health System Tracker. [cited 2020 Mar 22]; Available from: https://www.healthsystemtracker.org…
- Abrams A. Total Cost of Her COVID-19 Treatment: $34,927.43 [Internet]. Time. [cited 2020 Mar 22]; Available from: https://time.com…
- Khandelwal N, White L, Curtis JR, Coe NB. Health Insurance and Out-of-Pocket Costs in the Last Year of Life Among Decedents Utilizing the ICU. Critical Care Medicine 2019;47(6):749.
- Himmelstein DU, Campbell T, Woolhandler S. Health Care Administrative Costs in the United States and Canada, 2017. [Internet] Ann Intern Med; 2020. [cited 2020 Jan 9]; Available from: https://annals.org…
- Himmelstein DU, Woolhandler S. Public Health’s Falling Share of US Health Spending. Am J Public Health 2016;106(1):56–7.
- Report: Public health funding falls despite increasing threats [Internet]. Modern Healthcare; 2019. [cited 2020 Mar 19]; Available from: https://www.modernhealthcare.com…
- Leider JP, Coronado F, Beck AJ, Harper E. Reconciling Supply and Demand for State and Local Public Health Staff in an Era of Retiring Baby Boomers. Am J Prev Med 2018;54(3):334–40.
- Dolan J, Mejia B. L.A. County gives up on containing coronavirus, tells doctors to skip testing of some patients [Internet]. Los Angeles Times; 2020. [cited 2020 Mar 22]; Available from: https://www.latimes.com…
- Legido-Quigley H, Asgari N, Teo YY, et al. Are high-performing health systems resilient against the COVID-19 epidemic? [Internet] The Lancet; 2020. [cited 2020 Mar 7]; Available from: https://www.thelancet.com…
- Press A. Coronavirus: 38 test positive in New York City jails, including Rikers Island [Internet]. The Guardian; 2020. [cited 2020 Mar 22]; Available from: https://www.theguardian.com…
- Lander B. Doctors in NYC Hospitals, Jails, and Shelters Call on the City to Take More Aggressive Action to… [Internet]. Medium; 2020. [cited 2020 Mar 18]; Available from: https://medium.com…
- Zallman L, Finnegan KE, Himmelstein DU, Touw S, Woolhandler S. Implications of Changing Public Charge Immigration Rules for Children Who Need Medical Care. JAMA Pediatr 2019;e191744–e191744.
- U.S. Citizenship and Immigration Services. Public Charge [Internet]. USCIS; 2020. [cited 2020 Mar 15]; Available from: https://www.uscis.gov…
- Physicians for Human Rights, Human Rights First, Amnesty International USA. Re: COVID-19 and Immigrant Detention [Internet]. 2020. [cited 2020 Mar 22]; Available from: https://www.humanrightsfirst.org…
- Weber L. Coronavirus Threatens The Lives Of Rural Hospitals Already Stretched To Breaking Point [Internet]. Kaiser Health News; 2020. [cited 2020 Mar 22]; Available from: https://khn.org…
- Rovner J. In Coronavirus Relief Bill, Hospitals Poised To Get Massive Infusion Of Cash [Internet]. Kaiser Health News; 2020. [cited 2020 Mar 30]; Available from: https://khn.org…
- Lucas JH Elizabeth. ‘UVA Has Ruined Us’: Health System Sues Thousands Of Patients, Seizing Paychecks And Claiming Homes [Internet]. Kaiser Health News; 2019. [cited 2019 Nov 22]; Available from: https://khn.org…
- Himmelstein DU, Jun M, Busse R, et al. A Comparison Of Hospital Administrative Costs In Eight Nations: US Costs Exceed All Others By Far. Health Affairs 2014;33(9):1586–94.
- Lerner S. Big Pharma Prepares to Profit From the Coronavirus [Internet]. The Intercept; 2020. [cited 2020 Mar 15]; Available from: https://theintercept.com…
- Gaffney A, Lexchin J, The US/Canadian Pharmaceutical Policy Reform Working Group. Healing an ailing pharmaceutical system: Prescription for reform for United States and Canada. BMJ 2018;361:k1039.
- Holden E. US prescription drug supply chains face coronavirus stress test [Internet]. The Guardian; 2020. [cited 2020 Mar 23]; Available from: https://www.theguardian.com…
- Chidambaram P, Garfield R. Patterns in COVID-19 Cases and Deaths in Long-Term Care Facilities in 2020 [Internet]. Kaiser Family Foundation; 2021. [cited 2021 Aug 12]; Available from: https://www.kff.org…
- Powell R. Disability Activists Fight for the Right to Live in Their Communities [Internet]. Rewire News Group; 2018. [cited 2021 Aug 12]; Available from: https://rewirenewsgroup.com…
- Harrington C, Cassel C, Estes CL, Woolhandler S, Himmelstein DU. A National Long-term Care Program for the United States: A Caring Vision. JAMA: The Journal of the American Medical Association 1991;266(21):3023-3029.