Table of contents
Click the links below to jump to different sections of the newsletter. To view a PDF version of the shorter print edition of the newsletter, click HERE.
If you wish to support PNHP’s outreach and education efforts with a financial contribution, click HERE.
If you have feedback about the newsletter, email info@pnhp.org.
PNHP News and Tools for Advocates
- PNHP launches “Summer of Action” against Medicare profiteering
- Activists win resolutions against Direct Contracting/REACH in Seattle and Arizona
- APHA endorses single payer
- Dr. Rob Stone: My gift of stock is an investment in the future of Medicare for All
- PNHP Board nominations accepted during August
Research Roundup
- Data Update: Health care crisis by the numbers
- PNHP statement on abortion rights
- Studies and analysis of interest to single-payer advocates
PNHP Chapter Reports
- Arizona
- Colorado
- Georgia
- Illinois
- Kentucky
- Missouri
- New Jersey
- New York
- North Carolina
- Pennsylvania
- Vermont
- Washington
- West Virginia
PNHP in the News
PNHP News and Tools for Advocates
PNHP launches “Summer of Action” against Medicare profiteering
After several months of intense educating and organizing by PNHP and our allies, the Centers for Medicare and Medicaid Services (CMS) announced the termination of the controversial Medicare Direct Contracting model in February, admitting the program “did not align” with the Biden administration’s vision. At the same time, CMS said it planned to replace DC with a nearly identical program called “ACO REACH.”
CMS’ “rebranding” of Direct Contracting to REACH taught PNHP some important lessons. First, we knew that our work made an enormous impact — CMS would have never canceled the program if not for our campaign. But it wasn’t enough. We learned that we could never end Medicare profiteering unless we organize a powerful, national, grassroots movement.
To meet that challenge, PNHP expanded our organizing, working with chapter leaders to give dozens of presentations to community and senior groups. Along with our allies, we helped pass anti-DC/REACH resolutions in the Seattle City Council and the Arizona Medical Association.
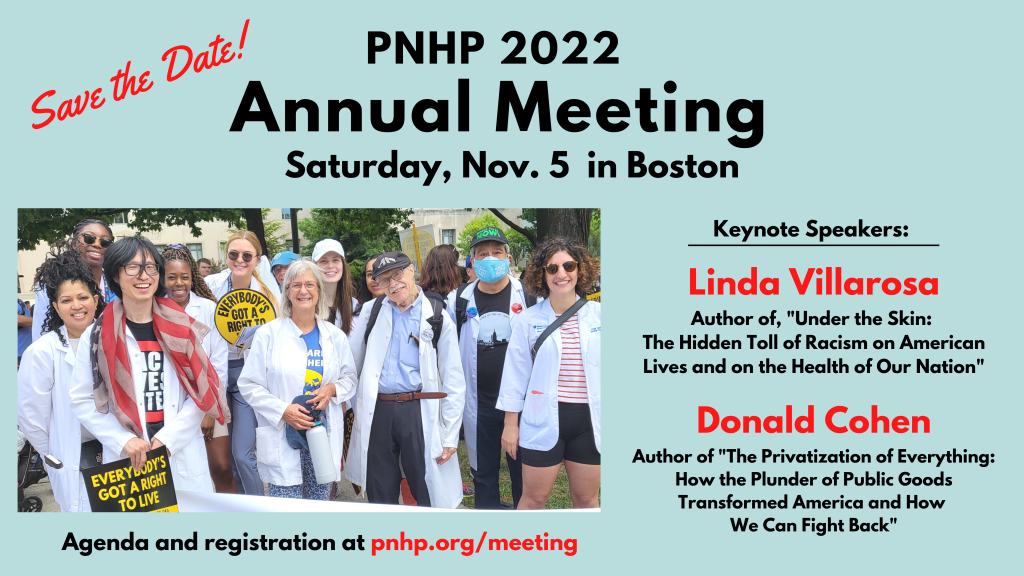
The organizing paid off. On May 23, PNHP hosted our biggest event ever: The launch of our “Summer of Action” against Medicare profiteering. More than 3,000 activists participated in this online event, where they learned the nuts-and-bolts of Direct Contacting and REACH, heard powerful testimonials from Medicare beneficiaries, and were inspired to take action by Congresswomen Katie Porter and Pramila Jayapal.
Anyone can get involved in our Summer of Action against Medicare profiteering. Here’s how:
- Call President Biden at (202) 456-1111 and demand he use executive action to end Direct Contracting and REACH (the White House switchboard is only open from 11 am – 3 pm ET on Tuesdays and Thursdays).
- Call your U.S. representative and senators using the U.S. Capitol Switchboard at (202) 224-3121, and demand they join the fight against Direct Contracting and REACH.
- Sign and share our petition against Medicare profiteering at ProtectMedicare.net/REACHPetition.
- Join our national Day of Action on July 30 (Medicare’s Anniversary). Contact organizer@pnhp.org to find out more.
Go to ProtectMedicare.net to find campaign updates, sample scripts, fact sheets, videos and more.
Activists win resolutions against Direct Contracting/REACH in Seattle and Arizona
Medicare advocates are celebrating two big victories in the movement to protect Medicare from profiteering and privatization.
In Seattle, seniors from the Puget Sound Advocates for Retirement Action, along with PNHP’s Washington Chapter, proposed a resolution against Medicare Direct Contracting and REACH. The resolution, which demands that the Dept. of Health and Human Services and President Biden immediately end Direct Contracting/REACH and protect Medicare from profiteering, was introduced by Councilmember Teresa Mosqueda and passed unanimously on April 26.
That same week, PNHP members Dr. Eve Shapiro and Dr. Michael Hamant introduced and successfully passed a similar resolution at the annual meeting of the Arizona Medical Association.

Drs. Shapiro and Hamant explained to their colleagues that since most physicians are now employed by large groups or health systems, they may find themselves practicing in Direct Contracting Entities (DCEs) without their knowledge or consent. Among concerns cited by the resolution is that “DCEs are allowed to keep as profit and overhead what they don’t pay for in health services, therefore giving them a dangerous financial incentive to restrict seniors’ care.”
The Seattle and Arizona resolutions are part of PNHP’s strategy to expand the fight against Medicare profiteering into every state and Congressional district in the nation.
APHA endorses single payer

After years of education and organizing by PNHP members, the 25,000-member American Public Health Association (APHA) strongly endorsed a Medicare for All policy at its most recent annual meeting, concluding that, “The most equitable and cost-effective health care system is a public, single-payer system.”
The policy statement was crafted by a working group of the APHA’s Medical Section, which included PNHP leaders Drs. Anthony Spadaro, Oli Fein, and Gordy Schiff, working with colleagues in the epidemiology, public health, pharmacy, and social work professions.
The working group published the position paper, “The American Public Health Association Endorses Single-Payer Health System Reform,” in the June 2022 edition of Medical Care, the official journal of the Medical Care Section of the APHA.
“The APHA is our nation’s strongest voice for public health, and I’m thrilled that my colleagues came together to support single payer as the solution to our fragmented and profit-oriented health system,” said Dr. Spadaro, a resident emergency medicine physician at the University of Pennsylvania and former board member of Students for a National Health Program.
The APHA resolution is part of PNHP’s Medical Society Resolutions campaign, which seeks to organize the medical profession by passing Medicare-for-All resolutions in every medical society in the U.S. The MSR campaign has passed resolutions in the American College of Physicians, the Society of General Internal Medicine, and the Hawaii, Vermont, New Hampshire and Washington state medical societies.
For more information on the PNHP Medical Resolutions Campaign, visit MedicalSocietyResolutions.org.
Dr. Rob Stone: My gift of stock is an investment in the future of Medicare for All
PNHP is known for its independence and unwavering commitment to a gold standard in health policy, in large part because of how we’re funded — by dues and donations of our members, never with corporate money that could compromise our mission.
This spring, longtime PNHP member Dr. Rob Stone discovered a new way to support PNHP’s mission: Through a generous gift of stock.
Dr. Stone, a palliative medicine physician, lives with his wife Karen in Bloomington, Indiana. He’s been a PNHP member since 2000, including roles as a board member and advisor, and usually donates about $1,000 per year to PNHP.
But when he turned 70 earlier this year, Dr. Stone began thinking more about his retirement and his legacy in the health justice movement. He’d been especially excited about PNHP’s campaign to stop Medicare privatization through Direct Contracting, and how important that was for the future of Medicare for All.
As he thought about how he could better support PNHP, Dr. Stone inherited Microsoft stock from his mother, who bought it in the 1980s; the stock had appreciated in value to about $40,000.
“I did the math and realized that if I sold the stock and kept it, I’d have to pay about $5,000 in capital gains taxes,” said Dr. Stone. “But if I donated the stock to PNHP, I would get a $40,000 tax deduction.”
What was more important was the incredible impact that his gift could make to PNHP’s mission.
“I’ve been very excited about the work that PNHP has been doing over the past year and was thrilled that I had an opportunity to help keep that momentum going,” Dr. Stone added. “My mother always encouraged me to give and to lead by example, and I’m hoping that my gift of stock will encourage other PNHP members to do the same.”
Part of Dr. Stone’s stock gift will support the Dorothy W. Stone Scholarship to help medical students attend PNHP’s Annual Meeting in November.
“I strongly encourage other members to think about donating stock to PNHP,” said Dr. Stone. “It’s easy. You get huge tax benefits, and you can make Medicare for All part of your legacy.”
PNHP Board nominations accepted during August
Nominations for PNHP’s Board of Directors will be open from August 1 to 31, with seats up for election in all regions and for at-large representation. Recent bylaws changes expands the number of seats on the Board, so that more members have the opportunity to serve on PNHP’s leadership team. The Board invites nominations and applicants from members interested in contributing to a diverse Board of Directors.
The following seats up for election for 2-year terms:
- At-large (1 seat)
- North East region (2 seats)
- South region (2 seats)
- North Central region (2 seats)
- West region (1 seat)
Questions about qualifications and expectations should be sent to deputy director Matthew Petty at matt@pnhp.org. Nominations (by self or others) are due to matt@pnhp.org by August 31, 2022. Ballots for electronic voting will be circulated in September 2022; please make sure your current email address is on the file with PNHP’s national office.
Research Roundup
Data Update: Health Care Crisis by the Numbers
Barriers to Care
Americans forego care due to cost: More than half of adults (51%) report that in the past year, they have delayed or gone without medical services due to costs, including 35% who put off dental services, 25% who put off vision care, and 24% who delayed general visits to their health provider. Kirzinger et al., “Health Tracking Poll March 2022: Economic concerns and health policy, the ACA, and views of long-term care facilities,” Kaiser Family Foundation, 3/31/2022
Cancer patients go into debt for care: More than half (51%) of U.S. cancer patients have gone into debt to cover the cost of care. Of those who incurred debt, 53% faced collections and 46% saw their credit scores drop; 62% have since delayed or avoided medical care, while half have sought the least expensive treatment options due to debt. In order to pay for cancer care, more than a quarter (28%) of patients depleted most or all of their savings, 28% have gone into credit card debt, 20% borrowed money from family and friends, and 11% took out another type of loan, like a payday loan or home refinancing. More than a third of cancer patients (36%) cut back on food, clothing, and basic household expenses. “Survivor Views: Cancer & Medical Debt, February 2022 Survey Findings Summary,” American Cancer Society, 3/17/2022
Women in the U.S. face worse health care and outcomes than peer countries: Nearly half (49%) of women of reproductive age in the U.S. skip or delay care because of costs, a rate more than double that of most peer nations. More than half (52%) of women in the U.S. report problems paying medical bills, compared to 10% in the U.K. Over one-quarter (27%) of American women spent $2,000 or more in out-of-pocket medical costs, as compared with less than 5% percent of women in the U.K., France, and Netherlands, and less than 10% in Germany, New Zealand, Canada and Norway. American women have the highest rate of avoidable deaths, and the U.S. maternal mortality rate is three times higher than France and seven times higher than Germany. Gunja et al., “Health and Health Care for Women of Reproductive Age: How the United States Compares with Other High-Income Countries,” Commonwealth Fund, 4/05/2022
Americans lack access to primary care: Compared to a set of 10 other wealthy nations, Americans are the least likely to have a longstanding relationship with a primary care provider, least likely to have access to home visits by a primary care provider, and are the least likely to be able to see a provider after regular office hours. The U.S also has the largest income gap between generalist and specialist physicians ($236,000 vs. $526,000 per year) and the highest medical school tuition. FitzGerald, “Primary Care in High-Income Countries: How the United States Compares,” Commonwealth Fund, 3/15/2022
High costs keep Medicare beneficiaries from critical treatments: Medicare Part D beneficiaries who did not receive subsidies to cap or lower their out-of-pocket costs were nearly twice as likely to not fill prescriptions for serious health conditions, since Part D drug costs can reach $10,000 or more. Among patients without subsidies, 30% did not fill their prescriptions for cancer drugs, 22% did not fill prescriptions for hepatitis C, and more than 50% did not fill therapies for high cholesterol or immune disorders. Dusetzina et al., “Many Medicare Beneficiaries Do Not Fill High-Price Specialty Drug Prescriptions,” Health Affairs, April 2022
Disparities plague drug affordability in Medicare: Among Medicare beneficiaries, 3.5 million seniors (6.6%) and 1.8 million under-65 adults with disabilities (22.7%) had difficulty affording their medications in 2019. Hispanic/Latinx and Black seniors were roughly 1.5 times more likely to have affordability problems compared to white seniors, and two times as likely not to get needed prescriptions due to cost. Among beneficiaries with diabetes, 10% of seniors and 26% of under-65 disabled adults reported medication affordability problems. Tarazi et al., “Prescription Drug Affordability among Medicare Beneficiaries,” U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation, Office of Health Policy, 1/19/2022
Health Inequities
Major racial disparities among cancer patients with COVID-19: Black cancer patients who were infected with COVID-19 had worse outcomes than similar white patients, with higher rates of hospitalization, intensive care unit admission, and mechanical ventilation. Black patients also experienced higher rates of lung, heart, and vascular complications, acute kidney injuries, and all-cause mortality, and were less likely to be treated with remdesivir and more likely to be treated with hydroxychloroquine. Fu et al., “Racial Disparities in COVID-19 Outcomes Among Black and White Patients with Cancer,” JAMA Network Open, 3/28/2022
Immigrants face major barriers to care: In 2020, more than one in four (42%) undocumented immigrants and 26% of documented immigrants were uninsured, compared to 8% of U.S. citizens. More than a quarter (28%) of undocumented children and 17% of documented children were uninsured, compared to 4% of children with citizen parents. The vast majority of immigrants (83%) were employed or lived with someone who was employed full-time (the same rate as citizens), but undocumented immigrants are not eligible for any kind of financial assistance through Medicaid coverage or tax credits. Income is also a barrier to care, as 44% of undocumented immigrants and 39% of documented immigrants are low-income, compared to 25% of citizens. “Health Coverage of Immigrants,” Kaiser Family Foundation, 04/06/2022
Coverage Matters
Diabetic amputations higher in states that didn’t expand Medicaid: Among patients of color that were hospitalized for diabetic foot ulcers in the two years after the implementation of the ACA, researchers found a 9% increase in major amputations in states that did not expand Medicaid, but no change in states that did expand. For uninsured adults, the amputation rate decreased 33% in expansion states but did not change in non-expansion states. Tan et al., “Rates of Diabetes-Related Major Amputations Among Racial and Ethnic Minority Adults Following Medicaid Expansion Under the Patient Protection and Affordable Care Act,” JAMA Network Open, 3/24/2022
Commercial Insurance: A Hazardous Product
Commercial insurers delay and deny care: Despite an agreement between the insurance industry and the AMA to streamline the prior authorization (PA) process, 84% of physicians report that the number of PAs required for prescriptions and medical services has increased over the last five years, with 65% saying that it is difficult to determine whether a prescription or medical service requires PA. Physicians report phone calls as the most common method for completing PAs (59%), with 45% of providers always or often using fax machines. An overwhelming majority (88%) of physicians report that PA interferes with continuity of care. “Measuring progress in improving prior authorization: 2021 Update,” American Medical Association, May 2022
High-deductible health plans (HDHPs) a major barrier to mental health care: When employers switched their employees into HDHPs, enrollees with depression were 18% less likely to seek outpatient care, those with ADHD were 15% less likely, and those with anxiety were 14% less likely. Inpatient hospital admissions also dropped significantly for HDHP enrollees with depression (19%), anxiety (16%), and ADHD (6%). After employers switched to HDHPs, overall plan spending for depression, anxiety, and ADHD dropped by $1,137, $984, and $868, respectively, but individual employees’ own spending increased by $326, $321, and $281, respectively. The switch to HDHPs also caused enrollees with anxiety or depression to skip preventative care such as breast, cervical, and prostate cancer screenings, as well as flu and pneumonia vaccinations. Fronstin and Roebuck, “How Do High-Deductible Health Plans Affect Use of Health Care Services and Spending Among Enrollees with Mental Health Disorders?” Employee Benefit Research Institute, 3/10/2022
Commercial insurers won’t pay for catheter supplies: Nearly 80% of catheter users with commercial insurance had to pay out-of-pocket (OOP) for catheters and catheter supplies, including 88% of those on UnitedHealthcare, 79% on BCBS, and 75% on Aetna, compared to 53% of those on public plans. Commercial plan enrollees paid more than three times the amount in OOP catheter expenses ($1,621) than those in public plans ($531). United Healthcare members faced the highest average OOP costs at $2,188 per year. “National Survey Among Catheter Users: A Study to Examine Catheter Usage and Catheter Coverage by Health Plan,” Spina Bifida Association and Duke Health, 3/16/2022
COVID survivors slammed with medical bills: Getting hospitalized for a serious case of COVID-19 left many commercially insured patients with bills averaging $1,600 to $4,000. More than one in ten patients (11%) with commercial insurance and 9.3% of patients with Medicare Advantage had more than $2,000 in bills in the first six months after a COVID-19 hospitalization. For patients hospitalized for pneumonia, OOP spending exceeded $2,000 for 12.1% with commercial insurance and 17.2% with Medicare Advantage plans. Chua, et al., “Out-of-Pocket Spending for Health Care After COVID-19 Hospitalization,” American Journal of Managed Care, 3/16/2022
Insurers celebrate record profits in early 2022: The six largest commercial insurers pocketed a combined $11.2 billion in the first three months of this year. UnitedHealth Group was the most profitable, reporting $5 billion in profit in the first quarter of 2022, followed by CVS Health (Aetna) with $2.3 billion, Anthem at $1.8 billion, Cigna at $1.2 billion, and Humana at $930 million. Minemyer, “UnitedHealth was this quarter’s most profitable payer—again,” Fierce Healthcare News, 5/9/2022
Insurance CEOs pocket millions in compensation: CEOs at the six largest commercial insurers earned nearly $115 million in combined total compensation last year. The late Michael Neidorff, former CEO of Centene, topped the list with $20.6 million in total compensation for 2021; followed by Karen Lynch of CVS Health (Aetna) at $20.4 million; Gail Boudreaux of Anthem with $19.3 million; David Cordani of Cigna with $19.9 million; Andrew Witty of UnitedHealth Group with $18.4 million; and Bruce Broussard of Humana with $16.5 million. Minemyer, “Centene’s Michael Neidorff was the highest-paid payer CEO last year. Take a look at what other execs earned,” Fierce Healthcare News, 4/27/2022
Privatizing Medicare and Medicaid
Commercial insurers drive up federal health spending: In 2020, commercial insurers’ overhead totaled $301.4 billion, up from $236.6 billion in 2019. Commercial Medicare Advantage plans accounted for $63.4 billion of that total, up 41.2% from 2019. The overhead of commercial insurers who run Medicaid managed care plans was $55.5 billion, up 64.9% from 2019. Hartman et al., “National Health Care Spending In 2020: Growth Driven By Federal Spending In Response To The COVID-19 Pandemic,” Office of the Actuary, CMS, published in Health Affairs, 12/21/2021
Medicare Advantage (MA) spending drags down Medicare budget in pandemic: Due to the sharp drop in utilization, 2020 spending on Part A and B services for Traditional Medicare (TM) decreased 5.8% from 2019, the first time annual spending has declined in more than 20 years. However, total Medicare spending increased because the federal government increased payments to commercial MA plans by 6.9%, since MA payments were determined in mid-2019 and not adjusted to reflect lower utilization. Biniek et al., “Traditional Medicare Spending Fell Almost 6% in 2020 as Service Use Declined Early in the COVID-19 Pandemic,” Kaiser Family Foundation, 6/1/2022
Medicare watchdog slams inflated Medicare Advantage costs: In 2020, Medicare paid 4% more for beneficiaries enrolled in MA than it would have if those beneficiaries were in Traditional Medicare. Medicare overpaid MA insurers by $12 billion just from upcoding alone. According to MedPAC, “The MA program has been expected to reduce Medicare spending since its inception … but private plans in the aggregate have never produced savings for Medicare, due to policies governing payment rates to MA plans that the Commission has found to be deeply flawed.” The Commission also noted that, “These policy flaws diminish the integrity of the program and generate waste from beneficiary premiums and taxpayer funds.” “Report to the Congress: Medicare Payment Policy,” Medicare Payment Advisory Commission, 3/15/2022
Medicare Advantage plans use prior authorization (PA) to deny needed care: An HHS watchdog found that among commercial MA plans’ PA denials, 13% were for services that met Medicare coverage rules and that the denials likely prevented or delayed necessary care. They also found that 18% of the MA plans’ denied payment requests met Medicare coverage rules and MA billing rules, and were thus improperly denied. “Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care,” U.S. Dept. of Health and Human Services Office of the Inspector General, 4/28/2022
Nearly half of seniors don’t understand limitation of MA plans: In a new survey, more than one-third (35%) of Medicare Advantage (MA) enrollees mistakenly believe they don’t have to stay in-network for care, while another 11% weren’t sure, and only half (50%) of MA enrollees said they understood that they don’t have free choice of provider. Grunebaum, “8 in 10 Rate Understanding of Medicare Advantage Good or Very Good: Survey,” MedicareGuide.com, 5/08/2022
Rampant health disparities among Medicare Advantage enrollees: Black, Indigenous and Alaska Native patients experienced the most significant disparities in clinical care among Medicare Advantage enrollees in 2021. American Indian and Alaska Native enrollees ranked lowest among all demographic groups for breast cancer screenings, respiratory conditions, and diabetes care. Compared to all MA enrollees, Black enrollees were less likely to receive follow-up care after emergency department visits for mental and behavioral health events, and also faced the most adverse prescribing practices, with clinicians more likely to dispense medications with significant side effects to Black people. Martino et al., “Disparities in health care in Medicare Advantage by race, ethnicicty and sex,” CMS Office of Minority Health, April 2022
High rate of “ghost” physicians in privatized Medicaid: In a study of four states from 2015 to 2017, researchers found that Medicaid managed care (or MMC, run by commercial insurers) provider network directories overstate how many physicians actually offer care to Medicaid enrollees. They found that 16% of adult primary care physicians listed in MMC networks qualified as “ghost physicians,” meaning they did not file any Medicaid claims in a year, and almost a third of MMC outpatient primary care and specialist physicians saw less than 10 Medicaid patients a year. Psychiatry was the specialty most likely to include ghost physicians, with 35% of MMC-contracted psychiatrists not seeing any Medicaid patients. Among all MMC-contracted providers, 25% of primary care doctors delivered 86% of the care, while 25% of specialists on average provided 75% of the care. Ludomirsky et al., “In Medicaid Managed Care Networks, Care Is Highly Concentrated Among a Small Percentage of Physicians,” Health Affairs, May 2022
Health Care for Profit
Surge in private equity (PE) in health care: Total PE investment in the health care industry has increased 20-fold, from $5 billion annually in 2000 to $100 billion in 2018. Annual PE acquisitions grew from 78 in 2000 to 855 in 2018. Appelbaum and Batt, “Private Equity Buyouts in Healthcare: Who Wins, Who Loses?” Institute for New Economic Thinking Working Paper Series, No. 118, May 2020
Private equity (PE) acquisition of hospitals leads to reduced staffing, higher profits: Between 2005 and 2014, hospitals acquired by PE firms saw a 1.78 percentage point increase in operating margins, along with a 2.79% decrease in bed count (about 4.43 beds). PE acquisition also reduced full-time equivalents (FTEs) staffing by 5.05%, an average loss of 36.97 FTE staff, with total nursing FTEs reduced by 4.38% or 10.52 FTE nurses. The ratio of outpatient to inpatient visits also decreased by 4.58%, indicating an increase in inpatient utilization likely due to more aggressive price negotiation for inpatient care with commercial insurers. Cerullo et al., “Financial Impacts And Operational Implications Of Private Equity Acquisition Of US Hospitals,” Health Affairs, April 2022
Higher nursing staff levels save lives: In a study of over 700,000 Medicare beneficiaries with sepsis, researchers found that an increase in registered nurse hours per patient day was associated with a 3% decrease in 60-day mortality, suggesting that hospitals that provide more RN hours of care could likely decrease sepsis deaths. Cimiotti et al., “Association of Registered Nurse Staffing With Mortality Risk of Medicare Beneficiaries Hospitalized With Sepsis,” JAMA Health Forum, 5/27/2022
Nursing home unions save lives: Nursing home labor unions were associated with 10.8% lower resident COVID-19 mortality rates, and 6.8% lower worker COVID-19 infection rates. Researchers estimate that 8,000 fewer resident deaths would have occurred if all nursing home staff were unionized during the pandemic, since labor unions were associated with better infection control policies and COVID-19 outcomes for essential workers. Dean et al., “Resident Mortality and Worker Infection Rates from COVID-19 Lower in Union Than Nonunion U.S. Nursing Homes, 2020–21,” Health Affairs, 4/20/2022
Investor-owned hospitals push more low-value care: “Low-value care” refers to medical services for which the potential for harm far outweighs the potential for benefit, such as spinal fusions for back pain, Pap smears for elderly women, and meniscus removal for degenerative knee joints. Researchers found that health systems that were primarily investor-owned performed more low-value care. In contrast, the systems that had the lowest levels of low-value care were those with a higher concentration of primary care physicians, a medical teaching program, and those that provide more uncompensated care. Segal et al., “Factors Associated with Overuse of Health Care Within U.S. Health Systems: A Cross-sectional Analysis of Medicare Beneficiaries From 2016 to 2018,” JAMA Health Forum, 1/14/2022
Nonprofit hospitals got big tax breaks with little charity care: Out of the 275 nonprofit hospital systems, 227 had “fair share deficits,” meaning they spent less on charity care and community investments than they received in tax breaks. Total “fair share deficits” amounted to $18.4 billion in 2019. The top five offenders were Providence Saint Joseph Health ($705 million more in tax breaks than it spent on charity care), Trinity Health ($671 million), Mass General Brigham ($625 million), Cleveland Clinic Health System ($611 million), and UPMC ($601 million). “Fair Share Spending: How much are hospitals giving back to their communities?,” Lown Institute, 4/12/2022
Majority of physicians now corporate employed: Physician practice acquisitions increased during the COVID-19 pandemic, and now nearly three out of four (74%) physicians are employed by hospitals, health systems, and other corporate entities such as private equity firms and health insurers. Nationally, hospitals and other corporations acquired 36,200 additional physician practices between 2019 and 2021, leading to a 38% increase in the percentage of corporate-owned practices. During that time, more than 108,000 physicians became employees of hospitals or other corporate entities (with 58,000 in hospitals and 50,500 in other corporate entities), a 19% increase. More than 75% of those employees (83,000) made the shift after the start of the pandemic. “COVID-19’s Impact on Acquisitions of Physician Practices and Physician Employment 2019-2021,” Avalere Health, April 2022
Pharma
Another year, another drug price hike: In early 2022, pharmaceutical companies raised wholesale prices by a median of 4.9% on more than 450 prescription medicines. United Therapeutics increased the price of its childhood cancer medication, Unituxin, by 9.9%, following a 9.9% increase in 2021 (it now retails for $14,349 per vial). Recordati raised the price of Neoprofen, a drug that treats premature infants at risk of a congenital heart defect, by 10% in 2020, 2021, and 2022 (it now retails for nearly $3,000). Leadiant hiked the price of a 50-year old cancer drug, Matulane, by more than 15% (it now retails for $11,969). Vertex raised the price of Trikafta, a cystic fibrosis medication that has no competitors and already has a list price of more than $311,000 for an annual supply, by 4.9% in 2022. Pfizer raised prices for roughly 100 drugs, including a 16.8% price hike for its injectable hydrocortisone product and a 6.9% increase on breast cancer drug Ibrance. Silverman, “Drug makers ring in the new year with 5% price hikes on hundreds of medicines,” 1/03/2022; “Brand Drug List Price Change Box Score,” 46Brooklyn Research, 1/05/2022
Drug prices outpace inflation: Half of all drugs covered by Medicare Part D (50% of 3,343 drugs) and nearly half of all Part B covered drugs administered by a physician (48% of 568 drugs) had price increases greater than inflation between July 2019 and July 2020. Among those drugs, one-third (668 drugs) had price increases of 7.5% or more. Among the most expensive price hikes were Eliquis, a blood thinner used by 2.6 million beneficiaries, with a 5.9% price increase; Revlimid, a treatment for multiple myeloma used by 44,000 beneficiaries, with a 6.5% increase; and Xarelto, a blood thinner used by 1.2 million beneficiaries, with a 4.1% price increase. Cubanski and Neuman, “Prices Increased Faster Than Inflation for Half of all Drugs Covered by Medicare in 2020,” Kaiser Family Foundation, 2/25/2022
PNHP statement on abortion rights
Studies and analysis of interest to single-payer advocates
“Response To: Cost-Sharing: Implications of a Well-Intended Benefits Strategy,” by Shannon M Rotolo, PharmD, BCPS, Journal of Managed Care and Specialty Pharmacy, May 2022. “United States could move toward a single-payer system with no premiums, no deductibles, and no copayments. Pharmacists in patient-facing roles would no longer need to provide support or coaching on health insurance literacy and no longer need to help patients choosing a plan that is “best” for them but potentially still inadequate. All patients would have consistent and transparent coverage from birth to death, regardless of their socioeconomic status.”
“Response to: A Potential Path to Universal Coverage With Medicare Advantage for All,” by Adam Gaffney, MD, MPH; David U. Himmelstein, MD; Steffie Woolhandler, MD, MPH. “Patients want good health care coverage and unrestricted choice of physicians and hospitals, not, as this Viewpoint suggests, choice of which insurance plan processes the bill. ‘MA for All’ would perpetuate the upward spiral of health care spending, divert more medical resources to insurers, and restrict choice. Far from looking to MA as a model for reform, we should question whether it should play any role at all.”
“Healthcare and Racial Justice: Systemic Change Is Needed for a More Equitable Health System,” by The Campaign for NY Health and the Black, Puerto Rican, Hispanic and Asian Legislative Caucus, 5/04/2022. Using New York State level data, the report found that Black Americans are 10% less likely than their white counterparts to hold employer-sponsored health coverage, and are also more likely to hold medical debt and to die from pregnancy-related causes. Black and Latinx Americans are less likely than white Americans to have jobs that permit remote work; and more likely to live in communities experiencing health provider shortages.
“Universal health coverage as hegemonic health policy in low- and middle-income countries: A mixed-methods analysis,” by Daniel Smithers, MD and Howard Waitzkin, MD, Social Science and Medicine, June 2022. Globally, the concept of “universal health coverage” (UHC) usually calls for public spending to buy health insurance from private corporations for those without insurance, as opposed to “Health care for all” (HCA), which provides the same comprehensive services for an entire population. UHC has become the dominant policy option favored by political and economic elites around the world, but further enhances the wealth and power of private corporations, without providing comprehensive services to all people.
“Universal healthcare as pandemic preparedness: The lives and costs that could have been saved during the COVID-19 pandemic,” by Alison P. Galvani, Alyssa S. Parpia, Abhishek Pandey, Pratha Sah, Kenneth Colón, Gerald Friedman, Travis Campbell, James G. Kahn, Burton H. Singer, and Meagan C. Fitzpatrick, PNAS, 6/13/2022. The fragmented and inefficient healthcare system in the U.S. leads to many preventable deaths and unnecessary costs every year, especially during a pandemic. Researchers estimate that a single-payer universal health care system would have saved 212,000 lives in 2020 alone, and also calculated that$105.6 billion of medical expenses associated with COVID-19 hospitalization could have been averted by a Medicare for All system.
“Medical Documentation Burden Among U.S. Office-Based Physicians in 2019: A National Study,” by Adam Gaffney, MD, MPH, Stephanie Woolhandler, MD, MPH, Christopher Cai, MD, David Bor, MD, Jessica Himmelstein, MD, Danny McCormick, MD, MPH, David U. Himmelstein, MD, JAMA Network, 3/28/2022. In this cross-sectional study, U.S. physicians spent a mean of 1.77 hours daily completing documentation outside office hours in 2019, and an estimated 125 million hours total documenting outside office hours. Nearly 57% percent of physicians said time spent documenting reduces the time they can spend with their patients. Relative to EHR users in other nations, U.S. physicians spend more time documenting in the EHR, with outpatient notes approximately times longer.
“COVID-19 Testing and Incidence Among Uninsured and Insured Individuals in 2020: a National Study,” by Adam Gaffney, MD, MPH, Steffie Woolhandler, MD MPH, and David U. Himmelstein, MD, Journal of General Internal Medicine, 2/09/2022. In 2020, uninsured adults (including many with chronic diseases) were less likely than the insured to have been tested for COVID-19 despite having higher rates of positive test results. Nearly one-third (32.8%) of the insured were tested compared to 26.2% of the uninsured. Among those tested, the positivity rate was almost double among uninsured (21.7%) relative to insured (11.1%) individuals.
“Health Care Debt In The U.S.: The Broad Consequences Of Medical And Dental Bills,” by Lunna Lopes, Audrey Kearney, Alex Montero, Liz Hamel, and Mollyann Brodie, Kaiser Family Foundation, 6/16/2022. Substantial shares of adults carry debt from medical and dental bills that they have paid off by taking on other forms of debt, including credit cards, personal bank loans, or loans from family and friends. The KFF Health Care Debt Survey finds that four in ten adults have some form of health care debt. Yet the likelihood of having health care debt is not evenly distributed. Uninsured adults, women, Black and Hispanic adults, parents, and those with lower incomes are especially likely to say they have health care-related debt.
PNHP Chapter Reports
Arizona
In Arizona, PNHP members Drs. Michael Hamant and Eve Shapiro successfully introduced and passed a resolution at the annual meeting of the Arizona Medical Association demanding that the Dept. of Health and Human Services and President Biden administration immediately end Medicare Direct Contracting and REACH. Drs. Hamant and Shapiro explained to their colleagues that since most physicians are now employed by large groups or health systems, they may find themselves practicing in DCEs without their knowledge or consent. To get involved in Arizona, contact Dr. Shapiro at evecshapiro@gmail.com.
Colorado
In Colorado, PNHP leaders helped to organize and host the One Payer States Meeting on May 21. The conference was co-sponsored by PNHP-CO, the Colorado Foundation for Universal Health Care and Health Care for All Colorado. To get involved in Colorado, contact Dr. Rick Bieser at rgbieser@gmail.com.

Georgia
In Georgia, a mix of new and experienced PNHP members — ranging from medical students to retirees — gathered in April to discuss single payer and celebrate the founding of three new Georgia Students for a National Health Program (SNaHP) chapters at Emory, Morehouse, and the Medical College of Georgia. In May, PNHP-GA assembled a Steering Committee to coordinate statewide education and organizing campaigns; the Committee’s first task is to work with allies like National Nurses United (NNU) to request that Georgia Senators Warnock and Ossoff co-sponsor the Senate single-payer bill. To get involved in Georgia, contact Dr. Elizabeth McCord at eomccord@gmail.com.
Illinois
In Illinois, Dr. Pam Gronemeyer of southern Illinois worked with allies in Missouri to pass a Medicare-for-All resolution in the St. Louis City Council (see Missouri report). PNHP-IL members worked with other local health advocates to protest the closing of CVS pharmacies in underserved neighborhoods; co-chair Dr. Anne Scheetz spoke at the coalition’s May 27 press conference in Chicago. To get involved in Illinois, contact Dr. Monica Maalouf at mmaalouf88@gmail.com.

Kentucky
In Kentucky, PNHP members have given presentations about Medicare for All to several candidates running for Congress, including one Republican. PNHP’ers have also been active in the campaign to protect Medicare from Direct Contracting and REACH by publishing opinion pieces in local news outlets and winning endorsements for the campaign from a number of Kentucky organizations, including the Kentucky AFL-CIO. To get involved in Kentucky, contact Kay Tillow at nursenpo@aol.com or Dr. Garrett Adams at kyhealthcare@aol.com.
Missouri
PNHP’s Missouri chapter spent much of the past year organizing a diverse coalition in support of a Medicare-for-All resolution in the St. Louis City Council. On March 4, Drs. Nat Murdock, Monique Williams, and Ed Weisbart presented the resolution to the City Council’s Black Caucus. Then on May 12, Dr. Weisbart, Angela Brown (CEO of the St. Louis Regional Health Commission), and patient advocate Chris Wilcox presented the resolution to the City’s Health and Human Services Committee, with a unanimous vote to support the resolution by both the committee and the full Board of Aldermen. To get involved in Missouri, contact Dr. Weisbart at pnhpMO@gmail.com.

New Jersey
In New Jersey, PNHP-NY Metro board member Dr. Leonard Rodberg made a presentation about Medicare Direct Contracting/REACH to the NJ Universal Healthcare Coalition meeting on April 23. The coalition is working to pass resolutions in the Medical Society of New Jersey, including a resolution supporting Medicare for All and a resolution opposing Direct Contracting/REACH. To get involved in New Jersey, contact Dr. Lloyd Alterman at lloydalterman52@gmail.com.
New York
In New York, PNHP’s New York-Metro chapter continues its monthly education forums; recent topics include pharmaceutical pricing, and abortion and reproductive health care in a post-Roe environment. NY-Metro held its annual Lobby Day on May 3, where advocates met with 13 state legislators to ask their support for the single-payer NY Health Act as well as the End Medical Debt Act, a new bill that would prohibit hospitals and insurance companies from placing liens on patients’ property or garnishing wages to pay medical debt. The chapter is also helping New York City public worker retirees fight the forced transition from Traditional Medicare to Medicare Advantage by urging NYC City Council members to sign a letter to the mayor asking him to keep the TM plan. On May 14, NY-Metro chapter members joined the “Bans Off Our Bodies” abortion rights march across the Brooklyn Bridge; several members provided medical support to marchers. This summer, the chapter is implementing a new communications strategy which includes publishing several letters and op-eds in local news outlets, as well as a social media campaign called #MedStoryMondays, where medical workers share their stories of how the current system has failed them or their patients. To get involved in New York, contact Mandy Strenz at mandy@pnhpnymetro.org.

North Carolina
Health Care Justice – NORTH CAROLINA in Charlotte held its annual membership meeting on March 31 with 70 health care advocates in attendance, including several elected officials. The group focused on the dangers of profiteering in Medicare through Direct Contracting/REACH. Chapter members participated in the May 14 “Bans Off our Bodies” rally for abortion care. Thanks to organizing by the North Carolina Medicare For All Coalition (a statewide coalition of 45 organizations), the North Carolina Democratic Party officially added single-payer Medicare for All to its platform at the party’s meeting on June 17. To get involved in Health Care Justice-NC, contact Dr. Jessica Schorr Saxe at jessica.schorr.saxe@gmail.com.
Health Care for All NC Raleigh members have been active in the Poor People’s Campaign, sending Medicare for All postcards to elected officials and sending a delegation of health care workers to the PPC Moral March in Washington on June 18. Chapter leaders have also been engaged in speaking events: Drs. Jonathan Kotch and Howard Eisenson spoke about single payer to faculty and trainees at Duke Medicine, and Jonathan Michels spoke to students at the Wake Early College of Health and Sciences who are now forming their own SNaHP chapter. To get involved in Health Care for All NC in Raleigh, contact Jonathan Michels at jonscottmichels@gmail.com.
Members of Healthcare For All – Western North Carolina in Asheville met with U.S. Senate candidate Cheri Beasley to urge her support for Medicare for All. Chapter leaders also hosted presentations on Medicare privatization through Direct Contracting and REACH at two large retirement communities in Asheville. To get involved in HCFAWNC, contact Terry Hash at theresamhash@gmail.com.
Pennsylvania
In Pennsylvania, PNHP’s Eastern PA chapter leader Dr. Walter Tsou gave a Grand Rounds on COVID-19, institutional racism, and health reform at Penn Family Medicine. Health Care for All Philadelphia participated in the annual “Mt. Airy Day” event where they explained their opposition to Medicare Direct Contracting and REACH to elected officials in attendance. To get involved in Pennsylvania, contact Dr. Tsou at macman2@aol.com.
Vermont

PNHP Vermont has given several presentations about the privatization of Traditional Medicare through Direct Contracting and REACH; several of these presentations have been recorded and broadcast on local access television stations. The PNHP Northern New England Summer internship just wrapped up with 13 medical students from Kentucky, Missouri, Arizona, Texas, Louisiana, Florida, New Jersey, New York, and Michigan. To get involved in Vermont, contact Dr. Betty Keller at bjkellermd@gmail.com or Ted Cody tscody@vermontel.net.
Washington
PNHP Washington has been very active in the campaign to stop Medicare privatization. Several of the chapter’s monthly educational forums have been focused on this topic, including a talk from Donald Cohen, author of “The Privatization of Everything,” as well as several training sessions on Direct Contracting and REACH. PNHP-WA worked closely with Puget Sound Advocates for Retirement Action, Health Care is a Human Right WA, and other allies to successfully pass an anti-DC/REACH resolution in the Seattle City Council. They also met with staff for U.S. Rep. Suzan DelBene, Sen. Maria Cantwell, and Sen. Patty Murray, urging them to fight back against DC/REACH. To get involved in Washington, contact pnhp.washington@gmail.com.
West Virginia
In West Virginia, PNHP and SNaHP members meet monthly to plan organizing tasks and discuss health care policy topics. Chapter members have given presentations about Direct Contracting/REACH to senior groups and will continue outreach to other health reform groups. Chapter leaders are actively recruiting new members at the state’s FQHCs with the goal of having at least one active member in each of the state’s 55 counties. To get involved in West Virginia, contact Dr. Dan Doyle at pnhp.wv@gmail.com.
PNHP in the News
News Items Quoting PNHP Members
“Seniors’ Medicare Benefits Are Being Privatized Without Consent,” The Lever, 4/11/2022, featuring Dr. Ed Weisbart and Kip Sullivan
“Secret Trump Program To Privatize Medicare Needs to End,” The Thom Hartmann Program, 5/02/2022, featuring Dr. Susan Rogers
“New Stealth Attack on Medicare Opens Door to Privatization,” Rising Up with Sonali, 5/24/2022, featuring Dr. Ana Malinow
- “Doctors, Lawmakers See Danger in Moving Medicare Toward Privatization,” ThinkAdvisor, 4/29/2022, featuring Drs. Ana Malinow and Ed Weisbart
- “St. Louis aldermen unanimously endorse national Medicare for All bill,” St. Louis Post Dispatch, 5/14/2022, featuring Dr. Ed Weisbart
- “Progressives Want End to Medicare Pilot,” Bloomberg, 5/24/2022, featuring PNHP
- “Biden Hikes Medicare Prices And Funnels Profits to Private Insurers,” The Lever, 6/01/2022, featuring Dr. Susan Rogers
- “Abortion Restrictions Force Medical Personnel To Commit Grave Ethical Violations,” Current Affairs, 7/01/2022, featuring Dr. Susan Rogers
Opinion pieces by PNHP members
- “Words of caution for Medicare beneficiaries,” by Dr. Robert Keifner, New Hampshire Union Leader, 4/25/2022
- “Anthem, MaineHealth both to blame for staggering costs,” by Dr. Lawrence Kaplan, Portland Press Herald (Maine), 4/23/2022
- “Our Healthcare System Is Making My Patients Sicker,” by Dr. Reena Agarwal, The River News, 4/28/2022
- “Beware the privatization of Medicare,” by Dr. Jay Brock, Fredericksburg FreeLance Star, 5/05/2022
- “The possible end of Medicare as we know it,” by Dr. Mary Alice Bisbee, Battleboro Reformer, 5/06/2022
- “Don’t fall for Joe Namath’s ads,” by Dr. G. Richard Dundas, Bennington Banner, 5/09/2022
- “Our health care system has too many barriers for Black, Indigenous, Latinx, Asian and poor New Yorkers,” by Dr. MaryLouise Patterson, Amsterdam News, 5/12/2022
- “Why Seniors Like Me Are Fighting Against Medicare Direct Contracting and ACO REACH,” by Rick Timmins, Common Dreams, 5/19/2022
- “Congress must stop the pillaging of traditional Medicare,” by Dr. Leonardo Alonso, Florida Times-Union, 5/20/2022
- “Medicare for all is a smart local issue for all to support,” by Dr. Pamella Gronemeyer, St. Louis Post Dispatch, 5/20/2022
- “It’s time for Albany to help New Yorkers in mental health crisis,” by Dr. Michael Zingman, AMNY (New York), 5/26/2022
- “Resist plan to privatize Medicare,” by Dr. Lawrence Eby, Albany Democrat Herald (Oregon), 5/27/2022
- “Just say ‘No, thank you!’ to DCE,” by Norma Morrison, Ph.D., Elizabethton Star (Tennessee) 5/31/2022
- “It’s time to rethink health care in U.S.,” by Dr. Richard McGowen and Lisa Jo Hubacher, Leader Telegram (Wisconsin), 6/02/2022
- “Medicare REACH program reaches into our pockets,” by Dr. William Orr, Albuquerque Journal, 6/21/2022
- “The Path to Health Equity Demands a Universal System,” by Drs. Monica Maalouf and Susan Rogers, Doximity, 6/29/2022