By Adam Gaffney, M.D.
Journal of Policy Analysis and Management, Point/Counterpoint, Winter 2018
Last summer, Republican efforts to repeal the Affordable Care Act (ACA)—seven-years in the making—dramatically collapsed. Yet, if the failed Senate vote in July marked a pause in conservative reform efforts, it only further animated the health care reform debate on the left side of the political spectrum. In this article, I argue that one of the reform models under discussion—single-payer national health insurance (NHI)—is the most potent and realistic policy solution.
First, I make the case that universal coverage is economically feasible. Second, I examine why achieving universal coverage remains paramount. Third, I describe how universal coverage can be quickly and effectively achieved via NHI enrollment. Fourth, I discuss benefit design, emphasizing the importance of comprehensive benefits, and first-dollar coverage. And finally, I explore the role of the public and private sectors, arguing that health care coverage must remain entirely within the public sphere if the goal of universal health care is to be, at long last, attained.
CAN WE AFFORD UNIVERSAL COVERAGE?
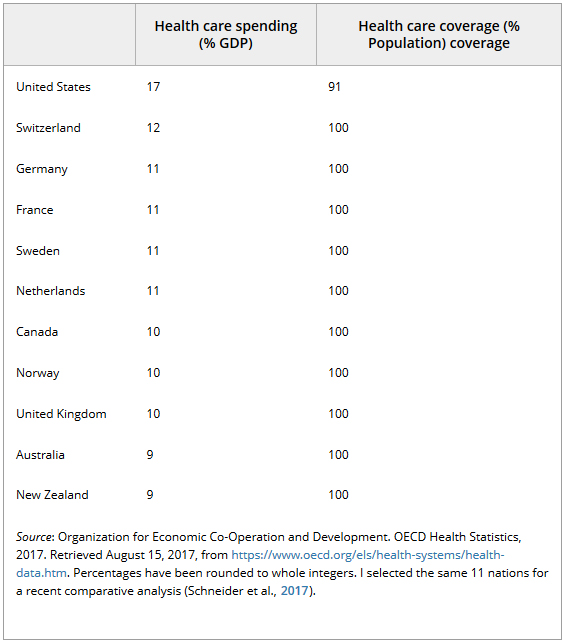
First: Can the United States afford universal coverage? Multiple lines of evidence demonstrate that we most certainly can. Table 1 provides estimates of population coverage, together with health care spending, for 11 OECD nations in 2015. While the United States is at the bottom of the list in terms of coverage, it is at the top of the list in terms of health care spending. A host of high-income nations have been able to achieve near 100 percent coverage despite their much lower levels of health care spending, and some of these nations—like Canada and the United Kingdom—have done this while eliminating cost sharing for most services.
Table 1. Health care spending and coverage in 11 OECD Nations, 2015
The experience of Taiwan—which implemented a NHI system in 1995—further bolsters the case for the affordability of universal health care. There, the costs of a rapid single-payer universal coverage expansion, and the resultant increase in health care utilization, were offset by other savings, such that the “total increase in national health spending between 1995 and 2000 was not more than the amount that Taiwan would have spent, based on historical trends” (Lu & Hsiao, 2003). Taiwan was thus able to implement a universal single-payer program with comprehensive benefits without an acceleration in national health spending growth, despite the fact that the nation began with a much higher baseline proportion of uninsured than the United States has currently (i.e., 43 percent vs. 9 percent 1) (Lu & Hsiao, 2003).
A back-of-the-envelope estimate further confirms the economic feasibility of universal coverage under NIH in the United States. A study of the cost of care for the uninsured found that for 2013, the uninsured used about half as much health care resources ($2,443) as the insured ($4,876) a year (Coughlin et al., 2014). These investigators used such figures to estimate that $121 billion was spent on the uninsured in 2013, suggesting that the uninsured might have been covered in that year for a similar (additional) sum. If we reduce that figure to account for the decline in the number of uninsured since 2013 and then inflate it for rising medical spending, we have a rough, back-of-the-envelope figure of $92 billion annually to cover all of the uninsured, including undocumented immigrants. 2
Though it may seem like a large sum, that figure represents only a small fraction of the savings that could be generated via the greater efficiencies of a single-payer system, discussed below. Together with evidence from other high-income nations abroad, it thus provides strong support for the affordability of universal coverage through NIH in the United States.
WHAT WOULD BE THE BENEFITS OF UNIVERSAL COVERAGE?
Even if we can afford universal coverage, is it worth the price? Though there has been some debate on whether coverage saves lives, a recently published review has strengthened the case that it indeed has such a protective effect (Woolhandler & Himmelstein, 2017a). For instance, the investigators note that three quasi-experimental difference-in-differences studies and most longitudinal observational studies support an association between coverage and reduced mortality, with an odds ratio of dying among the insured vs. the uninsured ranging from 0.71 to 0.97. And while the Oregon Medicaid experiment—the only randomized trial to examine the question (Finkelstein et al., 2012)—did not have a statistically significant protective effect on mortality, Woolhander and Himmelstein note that the direction of the effect was consistent with benefit, and in any event that the study was underpowered for this outcome.
Lowering mortality, of course, is not the only goal of universal coverage. Another review found that coverage had a beneficial impact on patient finances, health care access and use, the management of some chronic conditions, self-rated health, as well as on mortality (Sommers, Gawande, & Baicker, 2017).
It is worth noting that these sorts of benefits—especially on mortality—figured heavily in the debate over the repeal of the ACA. Yet, it is notable that every argument wielded against the repeal of the ACA on the grounds of lives lost also serves as a powerful argument for proceeding to universal coverage. For instance, it was estimated that under the Senate ACA repeal bill, 49 million would be uninsured by 2026 (Congressional Budget Office, 2017). However, 28 million are predicted to remain uninsured without the repeal. It seems hard to argue that having 49 million uninsured produces an unacceptable amount of unnecessary death and suffering, while leaving 28 million uninsured does not.
HOW DO WE GET EVERYONE ENROLLED?
While the goal of “universal coverage” today garners support from a diversity of voices, the devil is in the policy details. Against the single-payer approach advocated in this article, for instance, some argue for an incremental path to universal coverage by building on the ACA.
Perhaps the most prominent incremental reform is a “public option” plan added to the ACA marketplaces. However, it seems unlikely that such a reform would bring us towards universal coverage. While a public option might have lower premiums (Congressional Budget Office, 2013), it could potentially serve as something of a high-risk pool, enrolling sicker and most costly individuals, thereby raising premiums in the public plan while effectively subsidizing the profits of private insurers. Yet even assuming this could be avoided, there is no clear evidence that a public option would take us to universal coverage: The CBO’s 2013 scoring of a public option, after all, predicted that it would produce no significant reduction in the number of the uninsured (Congressional Budget Office, 2013).
A second proposed incremental approach to universal coverage would be to strengthen the ACA’s individual mandate. Some point to international examples—in particular, the Netherlands and Switzerland—to make this case. For instance, Herzlinger et al. assert that more “firm penalties” and a more “forceful approach” towards the individual mandate could achieve universal coverage in the United States (Herzlinger, Richman, & Boxer, 2017). They and others cite the example of Switzerland (which essentially has universal coverage), where penalties for being uninsured are more severe as compared to those of the ACA, and where those who misrepresent their insurance status can even be subject to imprisonment (Ginneken & Rice, 2015). Should we follow the Dutch and Swiss roads to universal coverage, for instance, by imposing a stiffer individual mandate penalty, instead of taking the single-payer path?
Absolutely not. After all, as Timothy Jost has written, not only are the Dutch and Swiss models often misrepresented, it is by no means clear that they are the best reform models to follow. The insurance plans sold in these nations are considered social services, not commodities (for this reason, the Dutch plans are not subject to European Union rules on competition, while in Switzerland, for-profit companies are barred from even selling basic plans) (Jost, 2009). But perhaps most critically, as Jost notes, the “managed competition” mandate-model reforms in both countries was not deployed to effect universal coverage, which had already been mostly achieved prior to the implementation of these reforms. And, critically, neither reform seems to have controlled costs, with Switzerland remaining the second most expensive health care system after the United States (Jost, 2009).
There are other reasons not to embrace these models. For instance, a 2015 study examining mandates in Germany, the Netherlands, and Switzerland found that even with these strict mandates, some remain uninsured, underinsured, or in default on their premiums (Ginneken & Rice, 2015). Premium defaulters and those who remain uninsured, moreover, are similar to the uninsured in the United States: they are more likely to be migrants, have low incomes, or be young, the study notes. These experiences cast doubt on using the ACA’s mandates to achieve universal coverage.
It is also worth noting that achieving universal coverage within a private-insurance framework may be prohibitively expensive. As will be later discussed, single-payer systems are capable of achieving much lower levels of administrative spending, savings needed to cover the cost of universal coverage.
Instead of a complicated patchwork approach, the most effective way to cover everybody would be instead to simply cover everybody through an NHI program. Some have suggested that enrolling everybody via a sweeping, quickly implemented “Medicare-for-all” system would entail a great deal of disruption. However, it is worth looking at the 1966 implementation of Medicare to see that this need not be the case. Medicare was signed into law by President Lyndon B. Johnson on July 30, 1965, and its benefits began on July 1, 1966, giving the Social Security administration less than a single year to enroll all of the nation’s seniors (Marmor, 2000, 87). And remarkably, it succeeded: by July 1, 1966, an overwhelming majority (18.9 million) of the nation’s 19.1 million seniors were enrolled in Medicare Part A, and more than 90 percent were enrolled in the voluntary “Part B” program (History of SSA During the Johnson Administration, 1963–1968; Marmor, 2000, 87). While it might be argued that times have changed—for instance, that Medicare’s administrators were dealing with a tabula rasa—this is not true. For instance, slightly more than half of seniors were enrolled in insurance plans prior to Medicare’s implementation (Davis, Schoen, & Bandeali, 2015, 9).
Finally, the example of Taiwan parallels that of Medicare. That nation also rapidly covered almost the entirety of the eligible population: Only 57 percent were covered before NHI’s implementation in 1995, vs. 96 percent by the end of the following year (Lu & Hsiao, 2003).
Such experiences provide firm evidence that when there is a will to universal coverage, there is a way.
WHAT WOULD BENEFIT DESIGN LOOK LIKE?
Single-payer proposals (Gaffney et al., 2016) and bills (H.R. 676, now sponsored by a majority of House Democrats) propose that comprehensive benefits—such as inpatient and outpatient care, dental care, long-term care, mental health care, and pharmaceuticals—be covered under NHI. This is essential for a number of reasons. First, these basic categories of benefits are required by all or nearly all at some point in the life course: There is no reason to relegate certain categories of medically-necessary services to the private insurance market. For instance, widespread lack of dental coverage—especially among the elderly and those of low income—produces unnecessary suffering, disability, and sometimes death, likely exacerbating social inequality in the United States (Otto, 2017).
Second, excluding important medical benefits from coverage may not only deprive individuals of important health care services, but in some instances may serve to increase rather than decrease health care spending. For example, though the single-payer Canadian Medicare system provides universal access to physicians’ services and hospital care, it does not provide universal access to prescription drugs. Yet this lack of public drug plan does not produce savings, but rather imposes costs, insofar as it leaves Canada with less leverage in drug price negotiations. According to one estimate, a universal public pharmaceutical plan might bring down total drug spending by 32 percent in Canada (Morgan et al., 2015).
Another benefit design issue relates to cost-sharing. At least since the RAND Health Insurance Experiment (HIE)—which found that imposing cost-sharing reduced health care utilization and spending without obvious harm to the health of the study population as a whole (Brook et al., 1983)—some have taken it as given that cost-sharing is a necessary and safe tool for cost containment. Yet evidence suggests that cost-sharing is not only unnecessary for cost control, but hazardous to health.
For instance, the RAND HIE itself found that cost-sharing might harm disadvantaged individuals, as it seemed to lead to higher blood pressure and hence potentially higher mortality (Brook et al., 1983). Moreover, cost-sharing has again and again been shown to reduce the use of both appropriate and inappropriate forms of health care (Brot-Goldberg et al., 2015), not surprising given that distinguishing the two reliably is generally thought to require a medical degree. Reducing the use of appropriate health care, in turn, can have adverse health consequences. For some children, for instance, cost-sharing reduces the use of asthma inhalers, and increases hospitalizations (Karaca-Mandic et al., 2012). And among adults with diabetes, high-deductibles reduce visits to specialists, and also increase visits to emergency rooms for diabetes-related complications (Wharam et al., 2017).
Cost-sharing is also unnecessary to control costs. For instance, for at least some specific types of health care (like medications after a myocardial infarction), the absence of cost-sharing may have a positive impact on health, and thus ultimately be at least cost-neutral (i.e., by reducing other forms of health spending) (Choudhry et al., 2011). But, additionally, as previously mentioned, some nations—like Canada and the United Kingdom—have abolished cost sharing while controlling health spending.
WHAT IS THE ROLE OF THE PRIVATE MARKET?
Under NHI, health providers can be a mix of public and (not-for-profit) private. However, health insurance should be entirely public, for a critical reason: The greater administrative simplicity produced by a single-payer is one of the key sources of savings to pay for universal coverage (Gaffney et al., 2016).
A body of literature supports the argument that public single-payers are more administratively efficient. For instance, whereas the administrative overhead of traditional Medicare is only 2 percent, that of private Medicare advantage plans is 11 percent, and that of total private insurance plans 13 percent (Davis, Schoen, & Bandeali, 2015, 23). The Taiwanese NHI, meanwhile, has startlingly (perhaps excessively) low administrative overhead, at little more than 1 percent of operating expenses (Cheng, 2015). And when looking beyond insurer overhead to total health system administrative costs (which include providers’ billing-related costs), it is notable that at least in 1999, 16.7 percent of Canadian health care dollars went to administrative activities, as compared to 31.0 percent in the United States (Woolhandler, Campbell, & Himmelstein, 2003).
As a result of such differences in administrative efficiency, the transition to a single-payer system might yield savings in excess of $500 billion a year, funds that could be then used to pay for the proposed system of comprehensive, first-dollar, equitable coverage for all (Woolhandler & Himmelstein, 2017b).
CONCLUSION
Some concede that single-payer NIH is the best policy option, yet point to the problem of political feasibility, noting that the prospects for sweeping reform at the national level, in the current climate, are slim. Yet, later or (one hopes) sooner, the political climate will change, opening the door for more progressive policy solutions, including those—like single-payer reform—that now seem farfetched.
It is also worth noting the political hurdles that would be encountered with more incremental reforms. For instance, a meaner individual mandate penalty is unlikely to serve politicians well as a rousing rallying cry. The mandate is perhaps the ACA’s most unpopular provision, supported by a mere 35 percent of Americans (Kirzinger, Sugarman, & Brodie, 2016). In contrast, majorities of poll respondents say they support “Medicare-for-all” (57 percent) and “single-payer” (53 percent) (Hamel, Wu, & Brodie, 2017).
Enrolling everybody in the nation into a single NHI program therefore remains the most efficient, effective, and perhaps most likely road to creating a right to health care in America.
ACKNOWLEDGMENTS
The author wishes to thank Professors David Himmelstein and Steffie Woolhandler for their years of mentorship, as well as for reading this manuscript.
The author is active in the not-profit organization, Physicians for a National Health Program, which advocates for single-payer reform. He has no financial conflict of interest with any relevant commercial entities.
1. Figures of the number of the uninsured in the United States throughout this article are from: National Health Interview Survey (Cohen, Zammitti, & Martinez, 2017).
2. The number of the uninsured is 36.2 percent lower now as a result of the ACA’s coverage expansion, or 28.6 million uninsured in 2016 vs. 44.8 million in 2013 (I assume a figure for 2017 that is unchanged from 2016). CMS’s National Health Expenditure tables show that per capita health spending rose from $9,110 in 2013 to a projected $10,833 in 2017, or an 18.9 percent increase. Thus, I reduced the $121 billion figure by 36.2 percent to account for the fall in the number of the uninsured, and then inflated it by 18.9 percent to account for rising medical spending. Of note, this approach to calculating the cost of covering the uninsured is somewhat similar (and relies on the same study of the cost of uncompensated care), but not identical, to that employed by a recent economic study on the cost of a single-payer bill for California, commissioned by supporters (Pollin et al., 2017).
BIOGRAPHY
Adam Gaffney is an Instructor in Medicine at Harvard Medical School, The Cambridge Hospital (e-mail: agaffney@challiance.org).
http://onlinelibrary.wiley.com…