Table of contents
Click the links below to jump to different sections of the newsletter. To view a PDF version of the shorter print edition of the newsletter, click HERE.
If you wish to support PNHP’s outreach and education efforts with a financial contribution, click HERE.
If you have feedback about the newsletter, email info@pnhp.org.
PNHP News and Tools for Advocates
- PNHP celebrates 35th anniversary
- PNHP welcomes new president Dr. Philip Verhoef
- Organizing team brings pediatricians into single-payer activism
Save the Date: Nov. 10-12 in Atlanta
Research Roundup
- Data Update: Health care crisis by the numbers
- Studies and analysis of interest to single-payer advocates
PNHP Chapter Reports
- California
- Georgia
- Kentucky
- Maine
- Missouri
- New Jersey
- New York
- North Carolina
- West Virginia
- Wisconsin
Protect Medicare Photo Petition
PNHP in the News
PNHP News and Tools for Advocates
PNHP celebrates 35th anniversary
This year, PNHP celebrates 35 years since its founding in 1988. In the decades since its beginning, our organization has grown from a small handful of physicians in a room in Massachusetts to over 26,000 members in chapters across the country, as well as thousands of medical students on dozens of campuses. During that time, we have cemented ourselves as leaders in the fight for health justice in the United States. Our ideas formed the intellectual foundation of the single-payer movement, and the Medicare for All bill as it exists today is a product of our expertise.
To commemorate these achievements and look forward to an even brighter future, PNHP has launched a 35th anniversary campaign, which kicked off with an activist meeting on February 23rd. Attendees new and old from across the organization came together to reminisce about their entrance into PNHP and the single-payer movement. Participants discussed our many recent accomplishments, such as successfully pressuring the Biden administration to freeze the REACH program and helping to pass single-payer resolutions in cities like Atlanta. At the end of the meeting, former president Dr. Susan Rogers and SNaHP leader Emily Huff laid out the plans for the year ahead.
The 35th anniversary campaign will go on throughout the year. First, we will use it to build support for the future of our movement, our SNaHP student activists. Next, we will dig deep on our efforts to protect Medicare from privatization, which threatens to kill Medicare for All before it has even started. Finally, we will use the campaign to greatly expand our circle of active physician members. Our efforts will culminate at the PNHP Annual Meeting in Atlanta on November 10-12, where we will convene with a much stronger and more formidable organization.
In order to make this initiative as successful as possible, we will need your help. Please go to pnhp.org/35years to learn more about our different fundraising and volunteer opportunities, including signing up to host a house party as well as starting a peer to peer fundraising campaign. We have an incredibly exciting year ahead of us, as we begin to build the power we need to finally win improved Medicare for All.
PNHP welcomes new president Dr. Philip Verhoef
Dr. Verhoef began his term as president in December of last year, taking over from past president Dr. Susan Rogers. He is an adult and pediatric intensivist, as well as a Clinical Associate Professor of Medicine at the John A. Burns School of Medicine at University of Hawaii-Manoa.
He first became interested in the movement in the late 2000s when working as a resident in California during a time when doctors were trying to get a single-payer bill passed in the state. Dr. Verhoef moved to Chicago and shortly thereafter joined up with PNHP-Illinois and the Illinois Single Payer Coalition, eventually becoming President of both groups. He joined PNHP’s national board as an adviser in 2014, and since then has been an integral part of our organizing and strategic efforts across the country.
At a time when we are on one hand facing threats to our public health care in the form of Medicare Advantage and REACH, and on the other seeing public interest and enthusiasm for single payer at its highest level ever, he is well poised to lead PNHP on both fronts. Under Dr. Verhoef, we will generate the widespread grassroots support and political power required to take on the insurance companies, build a base of allies, and finally win the health care system that all of us deserve. We would be remiss not to thank our immediate past president Dr. Susan Rogers for her indomitable leadership over the last few years, which has made PNHP a more powerful organization ready to meet these challenges. Please join us in giving her our gratitude, and welcoming Dr. Verhoef as our new president!

Organizing team brings pediatricians into single-payer activism
Pediatricians and medical students across PNHP’s membership have begun working on a campaign to bring more pediatricians into our movement, with the eventual goal of getting pediatric societies in America to endorse single payer as the only real solution to the health care problems that children and families face in this country. We interviewed Sam Accordino, a medical student and SNaHP member on the organizing team, to learn more about their work.

What drew you to the pediatric organizing campaign? I was drawn to this campaign because it presented an opportunity to advocate for the betterment of health care in America, particularly as it relates to that of children and families. I felt that this initiative was something that I had a passion for being involved with, as I have a particular interest in becoming a pediatrician in my future.
What are you most excited about working on in the campaign over the next few months? I am most excited about getting to collaborate with current pediatricians, while also learning about their experiences with health care and the ways that they became inspired to support this campaign.
Why should other pediatricians and medical students join the campaign? Other pediatricians and medical students should consider joining this campaign because it presents an involving and rewarding commitment to bettering the health of the children in America that we are empowered and dedicated to care for either now or in the future.
If you are interested in becoming a part of the pediatrics organizing team, please contact lori@pnhp.org!
Save the Date: Nov. 10-12 in Atlanta
Join us for PNHP’s in-person Annual Meeting, Leadership Training, and SNaHP Summit—scheduled for Nov. 10-12 in Atlanta.
We’ll convene for a weekend of single-payer workshops, plenary sessions, keynotes, and (most importantly) opportunities to meet with like-minded colleagues who are fighting for health justice across the U.S.

Research Roundup
Data Update: Health Care Crisis by the Numbers
Barriers to Care
Banning abortion would increase maternal mortality by 24%: A nationwide abortion ban would lead to an estimated additional 210 maternal deaths per year. Among non-Hispanic Black people, deaths would increase by 39%. Looking at only the states which have banned or are likely to ban abortion, maternal mortality increases vary, with some states seeing as much as a 29% increase. Stevenson et al., “The maternal mortality consequences of losing abortion access.” SocArXiv, 6/29/2022.
Americans are skipping therapy to save money: A third of American adults in therapy reported canceling a session due to out-of-pocket costs, and 48% of these adults say they would quit therapy altogether if costs increased. Among adults who stopped going to therapy, 22% cited the cost as a reason, and 15% cited changes of their insurance coverage. The average out-of-pocket monthly cost for therapy is $178, and reaches as high as $300 a session in some major cities. Ingram, “Cost Remains Significant Barrier to Therapy Access, Verywell Mind Survey Finds,” Verywell Mind, 5/9/2022.
Health care costs more concerning to Massachusetts residents than pandemic: Residents ranked the cost of care as three times as important as the pandemic. 42% of residents have put off care because of the cost, and 26% have put off purchasing prescription drugs. 80% believe it is extremely important to take action on health care costs, and 85% believe that the government should be doing more on this issue. Every age group and income bracket ranked cost as their most important issue in health care currently. Blue Cross Blue Shield of Massachusetts, “Massachusetts Residents Cite Health Care Costs, Not COVID, As Primary Health Care Concern,” 9/8/2022.
Americans are deeply dissatisfied with American health care: 56% of Americans believe that health care is handled poorly (defined as “not too well or not at all well”) in the United States. 74% believe that prescription medication costs are handled poorly, and 70% say the same about mental health care. Nearly 80% of Americans are at least moderately concerned about getting access to quality health care. This fear is especially pronounced among Black and Hispanic Americans, with almost 60% expressing extreme concern about access to quality care. Meanwhile, two-thirds of Americans view health care coverage as a government responsibility, and about 40% of Americans support a single-payer health care system. Seitz, “Americans give health care system failing mark: AP-NORC poll,” Associated Press, 9/12/2022.
Sexual assault survivors deal with extreme costs after seeking care: Emergency department costs for sexual assault survivors seeking medical care averaged $3,551. Survivors of sexual abuse during pregnancy faced the highest costs, at an average of $4,553. Just one-fifth of survivors seek out medical care after an assault, with fear of high costs being a likely contributor. 16% of these patients were expected to pay their bills out-of-pocket, and even individuals with employer-sponsored insurance paid an average of 14% of the total emergency visit cost. Dickman et al., “Uncovered Medical Bills after Sexual Assault,” New England Journal of Medicine, 9/15/2022.
1 in 10 individuals in the US has medical debt: 15.3% of uninsured individuals carry medical debt, compared with 10.5% of privately insured individuals. The mean amount of medical debt in 2018 was $21,687 per debtor. Factors such as hospitalization, disability, being on a high-deductible health plan, being on a Medicare Advantage plan, and having no insurance coverage were associated with a higher risk of having medical debt. Living in a Medicaid-expansion state was associated with a lower risk of medical debt. Losing insurance coverage, becoming newly disabled, and becoming newly hospitalized between 2017 and 2019 was associated with taking on medical debt by the latter year. Himmelstein et al., “Prevalence and Risk Factors for Medical Debt and Subsequent Changes in Social Determinants of Health in the US,” JAMA Network Open, 9/16/2022.
Adults with diabetes are skipping doses: More than 1.3 million Americans have skipped insulin doses, delayed purchasing the drug, or otherwise rationed it due to escalating costs. Around 16.5% of American adults with diabetes who need insulin did not take their dosage as prescribed due to financial considerations. Around 20% of younger adults have rationed insulin, as compared with 11% of adults 65 and older. Insulin rationing is higher among Black individuals compared to White and Hispanic individuals. Gaffney et al., “Prevalence and Correlates of Patient Rationing of Insulin in the United States: A National Survey,” Annals of Internal Medicine, November 2022.
Out-of-pocket spending in health care growing fast: In the United States, Out-of-pocket health care expenditures rose 10.4% in 2021, the highest rate in several decades. This increased spending was driven at least partially by demand for dental services, eyeglasses, and medical supplies. By contrast, overall health spending only grew by 2.7%, in large part due to a lower level of pandemic-related spending. Medicaid spending grew by 9.2%, Medicare spending by 8.4%, and employer health spending by 6.5%. Owens, “Out-of-pocket health costs spiked in 2021,” Axios, 12/15/2022.
Health Inequities
Access to in-school mental health services decreases for Black and Latino students in New Jersey: From 2008 to 2020, the statewide average of mental health professionals in public schools in New Jersey went from 8.2 per 1,000 students to 8.6 per 1,000 students. For White students, this number went from 7.4 to 8.5. However, the number of mental health professionals for Black students went from 10.3 to 8.5, and the number of professionals for Latino students went from 9 to 8.4. In general, the poverty rates for Black and Hispanic children in New Jersey are more than three times that of White or Asian children. Weber, “New Jersey’s Black Students Suffer a Decline in Access to School Mental Health Staff,” New Jersey Policy Perspective, 9/7/2022.
Racial disparities in mortality increase for many groups during the COVID-19 pandemic: With a few exceptions, almost all racial and ethnic groups across all ages saw an increase in their all-cause mortality rate compared to White individuals at the start of the pandemic, and during subsequent COVID surges. Before the pandemic, Black individuals of all ages had a mortality rate 1.19 times that of White individuals. During the initial wave of the pandemic, this rate increased to 1.77 times White individuals. For American Indian or Alaska Native individuals under age 65, all-cause mortality rates went from 1.74 times White individuals pre-pandemic to 2.25 times during the summer 2021 surge. While Asian and Hispanic populations had lower all-cause mortality rates as compared with White populations before the pandemic, these advantages shrank during the initial and subsequent COVID waves. Aschmann et al., “Dynamics of racial disparities in all-cause mortality during the COVID-19 pandemic,” PNAS, 9/20/2022.
Black Michiganders comprised 60% of Monkeypox cases in the state, but only 17% of vaccine doses: 70% of the doses of the Monkeypox vaccine in Michigan went to White residents. Although Detroit, a majority Black city, saw 38% of Michigan’s known monkeypox infections, with 102 of the state’s 265 identified cases, the first doses of the vaccine went to Oakland and Washtenaw counties. Shamus, “Black Michiganders got 60% of monkeypox cases, only 17% of vaccines,” Detroit Free Press, 9/29/2022.
Maternity care deserts increase in the United States: Since 2020, an additional 1,119 counties in the US have become maternity care deserts, areas with little or no access to maternity care services. Overall, more than 2.2 million women of childbearing age live in a maternity care desert, and more than 146,000 babies have been born in these deserts since 2020. Medicaid covers nearly half of births in maternity care deserts, compared with 40.1 percent in counties with full maternity care access. In 2020, 1 in 4 Native American babies and 1 in 6 Black babies were born in areas of limited or no access to maternity care services. “Nowhere to Go: Maternity Care Deserts Across the U.S.,” March of Dimes, October 2022.
Veteran care wait time disparities increase during pandemic: In the pre-pandemic era, Black and Hispanic veterans had waiting times which were on average 2.1 days longer and 1.3 days longer, respectively, than White veterans for orthopedic services. During the pandemic, wait times for both orthopedic and cardiology services increased for Black, Hispanic, and White veterans, with Black and Hispanic veterans seeing an overall greater increase in wait time in both categories. Black veterans saw mean wait time increases of 4.7 days for cardiology and 4.1 days for orthopedics, Hispanic veterans saw increases of 5.1 days for cardiology and 4.4 days for orthopedics, and White veterans saw increases of 4.5 days for cardiology and 3.8 days for orthopedics. Gurewich et al., “Disparities in Wait Times for Care Among US Veterans by Race and Ethnicity,” JAMA Network Open, 1/3/2023.
Coverage Matters
Out-of-pocket costs for Naloxone soar for uninsured patients: From 2014 to 2018, the average out-of-pocket cost for the opioid overdose reversal medication Naloxone decreased by 26% for insured patients, but increased by 606% for uninsured patients. This increase was even higher for some specific brands of the drug. From 2015 to 2016, the average out-of-pocket cost to uninsured patients for the brand Evzio rose 2429%. Peet et al., “Trends in Out-of-Pocket Costs for Naloxone by Drug Brand and Payer in the US, 2010-2018,” JAMA Health Forum, 8/19/2022.
Adults in Medicaid-enrolled families largely unaware of renewals resuming: 62% of adults with family Medicaid enrollment heard nothing at all about Medicaid eligibility redetermination and the coming end of the continuous coverage requirement. 16.2% of adults heard some about this issue, while 15.7% heard only a little. Just 5% of adults reported hearing a lot about future Medicaid renewals. Of those who had heard from a state agency or health plan about the upcoming change, only 21.3% were told how to get assistance with the process, and only 29% were informed of their options should they become ineligible for Medicaid. Haley et al., “Most Adults in Medicaid-Enrolled Families Are Unaware of Medicaid Renewals Resuming in the Future,” Urban Institute, 11/15/2022.
Young adults in Medicaid-expansion states see improved cancer survival: In states that expanded Medicaid, two-year overall survival for young adult cancer patients rose from 90.4% to 91.9%. In states that did not expand Medicaid, survival increased from 89% to 90.1%, giving the Medicaid-expansion states an advantage of around 0.4%. Survival rate increases associated with Medicaid expansion were concentrated by type in female breast cancer and by stage in patients with stage IV disease. Ji et al., “Survival in Young Adults With Cancer Is Associated With Medicaid Expansion Through the Affordable Care Act,” Journal of Clinical Oncology, 12/16/2022.
Fewer postpartum hospitalizations in states that expanded Medicaid: The rate of hospitalizations of either the newborn baby or mother in the first 60 days following birth decreased by 17% in states that expanded Medicaid. Approximately 75 percent of this decrease can be attributed specifically to a smaller number of childbirth-related hospitalizations. The rate of hospitalization between 61 days and six months after birth decreased by 8% in Medicaid-expansion states as well. Steenland and Wherry, “Medicaid Expansion Led to Reductions in Postpartum Hospitalizations,” Health Affairs, January 2023.
Millions set to lose Medicaid coverage as public health emergency ends: As the government winds down the Medicaid continuous coverage requirement, millions of Americans may lose their coverage either through ineligibility or by falling through the cracks of the renewal process. Anywhere between 5 and 14 million Americans could be kicked off their current Medicaid coverage, with the federal government estimating 6.8 million people will lose coverage despite still being eligible under Medicaid requirements. In the years since the pandemic began, the number of Americans on Medicaid and CHIP, the Children’s Health Insurance Program, grew by almost 20 million, to a total enrollment of 90.9 million. Yu, “6.8 million expected to lose Medicaid when paperwork hurdles return,” NPR, 1/24/2023.
Commercial Insurance
Patients with chronic diseases face substantially higher financial difficulties: Comparing commercially insured individuals with no chronic conditions to those with 7-13 chronic conditions, the latter group had higher probabilities of having medical debt in collections (7.6% vs 32%), delinquent debt (14% vs 43%), and a low credit score (17% vs 47%). Among those with medical debt in collections, the estimated amount owed for those with several chronic conditions was also significantly higher ($784 vs $1252). Becker et al., “Association of Chronic Disease With Patient Financial Outcomes Among Commercially Insured Adults,” JAMA Internal Medicine, 8/22/2022.
Claim denials and delayed insurer payments increasing: 67% of healthcare leaders have seen an increase in denied claims in the past year, compared with 33% of leaders who saw an increase in denied claims in 2021. In hospitals, the initial claim denial rate increased from 10.2% in 2021 to 11% in 2022. Denial value went from 1.5% of health systems’ gross revenue in January 2021 to 2.5% in August 2022. Providers are also waiting longer for payment from insurers, with the proportion of claims taking more than 90 days after reception to be paid rising from 32% in January 2021 to 37% in August 2022. Deveraux, “Health systems see increasing claim denials as payer ‘delay tactic,’” Modern Healthcare, 11/21/2022.
Lack of competition in health insurance markets: Health insurance giants dominate the market in the United States, and are gaining even more control. 75% of metro areas lacked a competitive market for commercial insurance, compared with 73% the previous year. In 91% of regions, one insurer controlled at least 30% of the market. When it came to Medicare Advantage, a single carrier enrolled more than half of beneficiaries in 34% of markets. In most states, two insurers hold at least 50% of the overall market share. Tepper, “Health insurance markets lack competition, AMA reports,” Modern Healthcare, 11/1/2022.
Profiteers in Health Care
Private equity’s takeover of medicine continues: In 2021, private equity firms spent over $200 billion on more than 1,400 health care acquisitions. Companies owned or managed by these firms have paid fines of more than $500 million since 2014 to settle at least 34 lawsuits under the False Claims Act. Some specialties, such as anesthesiology and gastroenterology, have been largely taken over by private equity, while regulators ignore the more than 90% of private equity investments that fall below the government’s $101 million antitrust review threshold. Schulte, “Sick Profit: Investigating Private Equity’s Stealthy Takeover of Health Care Across Cities and Specialties,” Kaiser Health News, 11/14/2022.
Vaccine producers keep billions in payments for canceled doses: Gavi, the humanitarian vaccine organization, purchased Covid vaccines from drug companies as part of its global vaccination program known as Covax. These companies together made $13.8 billion from the vaccines distributed through the program so far, but they refuse to return the $1.4 billion paid for vaccine orders that have since been canceled as the program winds down. Novavax, for example, is refusing to refund $700 million for vaccines it never gave to the program. Nolen and Robbins, “Vaccine Makers Kept $1.4 Billion in Prepayments for Canceled Covid Shots for the World’s Poor,” New York Times, 2/1/2023.
Nursing home owners paid themselves millions while residents suffered: Of the more than 600 nursing homes in New York, almost half hired companies run or controlled by their owners to perform various services, paying themselves well above market rates while the federal government doled out millions of dollars of pandemic relief money to those same homes. Together, these corporations made profits of $269 million on an average margin of 27%, while conditions in homes steadily deteriorated among staff shortages and scores of deaths from COVID and other illnesses. Rau, “Nursing home owners drained cash while residents deteriorated, state filings suggest,” NPR, 1/31/2023.
Medicare and Medicaid Privatization
Department of Justice joins False Claims Act lawsuit against Cigna: The suit was filed in 2017 by a service provider for Cigna’s Medicare Advantage (MA) subsidiary. Cigna is accused of using improper diagnosis coding to cheat the government out of $1.4 billion during the years 2012-2019. The codes used to collect this money allegedly did not reflect the actual condition of patients, and diagnoses lacked the testing and imaging information necessary to prove the existence of the ailments. Moreover, the beneficiaries did not receive treatment for the conditions that were reported on the diagnostic codes. Kacik, “DOJ joins Cigna Medicare Advantage Fraud Case,” Modern Healthcare, 8/25/2022.
Centene settles overcharging allegations with 14 states: The company, which is the nation’s largest Medicaid managed care operator, has reached settlements with these states to resolve allegations of overcharging state Medicaid programs for prescription drugs. These settlements to date have totaled over $800 million dollars in the following states: California, Texas, Ohio, Indiana, Illinois, Mississippi, Iowa, Kansas, New Hampshire, Washington, Oregon, Massachusetts, New Mexico, and Arkansas. The largest settlements thus far have been in California ($215 million), Texas ($165 million), and Ohio ($88 million). Liss, “Centene reaches $215M settlement with California,” Healthcare Dive, 2/9/2023.
Big Insurers expanding Medicare Advantage plans in 2023: Aetna is expanding its MA offerings from 1,875 counties to 2,014 counties. UnitedHealthcare is growing from 2,629 counties to 2,798 counties. Elevance Health, formerly Anthem, which has more than 1.6 million MA beneficiaries, is expanding into 210 new counties. Cigna will expand from 477 counties to 581 counties, and Humana will expand to 140 new counties. Jaspen, “Big Health Insurers Will Expand Medicare Advantage to Hundreds of New Counties for 2023,” Forbes, 10/1/2022.
Government audits uncover millions in Medicare Advantage overpayments: 90 audits which examined billings from 2011 through 2013 uncovered around $12 million in net overpayments for the care of just over 18,000 patients. 71 audits uncovered net overpayments, and 23 audits showed overpayments of over $1,000 per patient on average. UnitedHealthcare and Humana accounted for 26 of the 90 audits. Schulte and Hacker, “Audits – Hidden Until Now – Reveal Millions in Medicare Advantage Overcharges,” Kaiser Health News, 11/21/2022.
Medicare Advantage plans associated with higher mortality for complex cancers: For patients undergoing surgery for cancers located in the lungs, esophagus, pancreas, stomach, liver, and rectum, enrollment in an MA plan was associated with a lower probability of treatment in a high-volume hospital with physicians experienced in treating complex cancers. Compared with patients in Traditional Medicare, patients in MA with stomach and liver cancer were 1.5 times likelier to die within a month after their surgeries, and patients with pancreatic cancer were twice as likely to die in the same time frame. Patients on Traditional Medicare were more likely to be treated at a teaching hospital (23% vs 8%), a hospital accredited by the Commission on Cancer (57% vs 33%), or a National Cancer Institute-designated cancer center (15% vs 3%). Raoof et al., “Medicare Advantage: A Disadvantage for Complex Cancer Surgery Patients,” Journal of Clinical Oncology, 11/10/2022.
New audits in Medicare Advantage will recoup hundreds of millions in overpayments: The audits will proceed under a new rule finalized by the Biden administration. The first year of audits will cover 2018 plans, from which the government estimates it will get back $479 million from MA insurers. Over the next decade, from 2023 to 2032, this number is expected to increase to $4.7 billion, which is overall higher than the previous estimate of $381 million per year from annual audits. Herman and Bannow, “Medicare Advantage insurers to repay billions under final federal audit rule,” STAT News, 1/3/2023.
MA plans denying inpatient claims at greater rates: Inpatient claim denial rates for MA plans through November 2022 stood at 5.8%, as compared with 3.7% for all other payer categories. Looking just at payers within MA, providers wrote off 8.5% of inpatient revenue as uncollectible in 2022, up from 4.7% in 2021. In terms of overall revenue, providers wrote off 3.6% as uncollectible in 2021 and 5.9% as uncollectible in 2022. Many MA plans have adopted strict criteria for authorization which has led to this increased rate of inpatient denial. Lagasse, “Medicare Advantage plans denying more inpatient claims,” Healthcare Finance, 2/21/2023.
Pharma
Online prescriptions drive huge pharmaceutical profits: An explosion in telehealth has led to increased prescription of drugs through the internet, with one prescribing service estimating that more than 90% of eligible patients who finish their intake forms get a prescription for the drug they clicked on. The drug industry spends $25 billion a year on marketing, and has recently increased its direct-to-consumer ad spending as a result of this newfound wave of telehealth prescriptions. Between 1997 and 2016, online direct ad spending by pharmaceutical companies increased by around $500 million. Palmer, “‘This is pharma’s dream’: How drugmakers are turning telehealth into a marketing gold mine,” STAT News, 9/14/2022.
High drug prices are not justified by research and development costs: For 60 drugs approved by the FDA between 2009 and 2018, there was no correlation between estimated research and development investments and drug costs at launch, 1 year after launch, or in the year 2021. These drugs accounted for 17.7% of all drugs authorized by the FDA over the period. The idea that high prices are needed to make back the money spent on creating the drug is thus unsupported by data. Wouters et al., “Association of Research and Development Investments With Treatment Costs for New Drugs Approved from 2009 to 2018,” JAMA Network Open, 9/26/2022.
Drugmakers raising prices on a large group of medications: Companies including Pfizer, GlaxoSmithKline, and Sanofi are expected to raise prices on more than 350 drugs in 2023. These price increases come after pharmaceutical companies already raised prices on more than 1,400 drugs in 2022, the most since 2015. The average increase in drug prices was 6.4% in the previous year. Some drugs with planned price increases include the shingles vaccine Shingrix (7%), the CAR-T cell therapies Abecma and Breyanzi (9%), and the autoimmune treatment Xeljanz (6%). Erman and Steenhuysen, “Exclusive: Drugmakers to raise prices on at least 350 drugs in U.S. in January,” Reuters, 12/30/2022.
Novel drugs are debuting at record high prices: The median annual price for drugs newly approved by the FDA in 2022 is $222,003. The median in the first half of the year was $257,000, and the median in the second half was $193,900. One of the drugs approved in the second half of 2022, a one-time gene therapy known as Hemgenix, is the most expensive drug in history at $3.5 million. The average price of a newly launched cancer drug in 2021 was $283,000, up 53% from the average price in 2017. Beasley, “U.S. new drug price exceeds $200,000 median in 2022,” Reuters, 1/5/2023.
Studies and analysis of interest to single-payer advocates
“Arizona’s debt collection reform – a small step towards health justice,” by Christopher Robertson; Steffie Woolhandler; David U Himmelstein, The BMJ, 11/23/22. “US patients can incur medical debt either because they lack health insurance coverage (11.4% of Arizonans; 8.6% of Americans nationwide) or because their insurance policies leave them exposed to substantial costs through deductibles and co-payments, which federal law allows to be as high as $15,000 a year for families. As a result, Americans carry a total of at least $88bn in medical debt, and it’s the most common adverse item on credit reports.”
“Hospital Expenditures Under Global Budgeting and Single-Payer Financing: An Economic Analysis, 2021-2030.” by Adam W. Gaffney; David U. Himmelstein; Steffie Woolhandler; James G. Kahn, International Journal of Social Determinants of Health and Health Services, 1/30/23. “We estimate that non-federal hospital operating budgets will total $17.2 trillion between 2021 and 2030 under current law versus $14.7 trillion under single-payer with global budgeting.”
“LIFE AND DOLLARS: a health care insider’s account of how prior authorization really works.” Anonymous, HEALTH CARE un-covered, 1/30/23. “By having prior authorizations in place, did anything actually improve in your overall patient population? The answer is probably no, because the purpose of prior authorizations is to save dollars, not improve patient outcomes, regardless of what they say.”
“Accountability for Medicare Advantage Plans is long overdue.” by Physicians for a National Health Program, 3/1/2023. “The long unbroken record of gaming the payment system and overpayments to MA plans without evidence for improved outcomes (and easily gamed quality metrics do not qualify as evidence of improvement) point to the folly of expecting capitated fiscal intermediaries to reduce Medicare cost.”
“Chronic Illness in Children and Foregone Care Among Household Adults in the United States: A National Study,” by Narm, Koh Eun M.D., M.S.; Jenny Wen, M.D., M.P.H.; Lily Sung, M.D., M.S.; Sofia Dar, M.D.; Paul Kim, M.D.; Brady Olson, M.D.; Alix Schrager, M.D.; Annie Tsay, M.D.; David U. Himmelstein, M.D.; Steffie Woolhandler, M.D., M.P.H.; Natalie Shure, M.A.; Danny McCormick, M.D.; Adam Gaffney, M.D., Med Care, 4/1/2023. “Adults living with children with chronic illnesses may sacrifice their own care because of cost concerns. Reducing out-of-pocket health care costs, improving health coverage, and expanding social supports for families with children with chronic conditions might mitigate such impacts.”
PNHP Chapter Reports
California
In California, PNHP-CA members across various chapters have been busy with a myriad of initiatives. PNHP-Ventura led a successful effort to get the City Council of Ojai to pass a resolution in support of single payer. During the recent open enrollment period, organized groups of PNHP-Humboldt County members attended Medicare Advantage information sessions, using questions to expose the deficiencies of MA programs and urge seniors in attendance not to sign up. PNHP-Napa convinced Congressman Mike Thompson to write to Secretary Becerra and ask him to terminate REACH. Finally, PNHP Bay Area organized a webinar on building business support for single payer. Members of all chapters have also been presenting on single payer at a variety of conferences, CME sessions, and Grand Rounds.
To get involved in California, please contact Dr. Nancy C. Greep at ncgreep@gmail.com.

Georgia
In Georgia, PNHP members hosted a Fall Social at Manuel’s Tavern in Atlanta. Over 15 chapter members joined the event, and shared stories about their lived experiences with our failing health care system. Steering Committee members Belinda McIntosh and Henry Kahn collaborated with the Florida PNHP chapter on various outreach efforts, strengthening the relationship between the two groups. Finally, the chapter engaged with members of the Atlanta City Council prior to their historic passing of a resolution supporting the Congressional Medicare for All bill HR 1976.
To get involved in Georgia, please contact Dr. Elizabeth McCord at eomccord@gmail.com.
Kentucky
In Kentucky, members of Kentuckians for Single Payer Healthcare (KSPH) produced weekly radio shows, interviewing physicians and others on issues related to local health care, VA care, value-based payments, and Medicare privatization. Two of the shows featured members of the Board of Supervisors in Dunn County, Wisconsin, and Dr. Pam Gronemeyer in southern Illinois, on their successful Improved Medicare for All ballot questions. Several members participated in the presentation of a Grand Rounds on health care systems sponsored by the Greater Louisville Medical Society for the Kentucky Medical Association. In December, KSPH hosted a virtual webinar on Medicare Privatization and ACO REACH featuring Dr. Corinne Frugoni, past president of PNHP-CA. Finally, members worked to get union and central labor council resolutions passed calling for an end to ACO REACH.
To get involved in Kentucky, please contact Kay Tillow at nursenpo@aol.com or Dr. Garrett Adams at kyhealthcare@aol.com.
Maine
In Maine, members worked on a campaign to endorse candidates for the state legislature and recognize those who support the mission to bring universal single-payer health care to all Maine residents. In addition, the chapter launched a weekly series of Lunch and Learns for Maine legislators, with speakers from current and former members of Maine AllCare as well as the related 501(c)(4) organization Health Care for All Maine. Finally, members of the chapter are participating on a committee of the Maine Medical Association to update their statement on health reform, with the goal of achieving an endorsement of language around single payer and universal health care.
To get involved in Maine, please contact Karen Foster at kfoster222@gmail.com.
Missouri
PNHP members in Missouri held a Zoom meeting to discuss several items mainly related to efforts to educate people across the state about single-payer health care. They talked about whether and how PNHP strategies might be applied in the state, how best to utilize the documentary “American Hospital,” and possibilities for an online book club. Several members have also committed to making calls to get lapsed members back into the organization. Even without in-person gatherings, the chapter continues to work on building power and advocating for fundamental health care reform in Missouri.
To get involved in Missouri, please contact Dr. Ed Weisbart at missouri@pnhp.org.

New Jersey
The New Jersey chapter, also known as the NJ Universal Health Care Coalition, conducted a poll in collaboration with the Rutgers University Eagleton Center for Public Interest Polling which found that 70% of New Jersey voters support Medicare for All. In addition, members of the chapter met with Congresswoman Mikie Sherill to express their strong opposition to the REACH program (part of a larger campaign of writing letters to all NJ legislators informing them of the issue). Dr. Lloyd Alterman also had a letter to the editor on ACO REACH published in the state’s largest paper, the Star Ledger.
To get involved in New Jersey, please contact Dr. Alterman at lloydalterman52@gmail.com.
New York
In New York, PNHP-NY Metro Chapter is helping to build power through its inaugural cohort of the Universal Healthcare Legislative Advocacy Fellowship. This nine month program is intended for students and providers new to the movement, and focuses on building a set of advocacy and organizing skills that will enable them to become leaders in organizing efforts like the push for the NY Health Act. The chapter also held a picnic in Central Park to welcome new students to their programs and do outreach for the fellowship program as well as the Annual Meeting. Finally, the chapter is continuing to support the campaign against the city’s attempt to move retirees onto a Medicare Advantage plan – in particular, they have helped allies to develop strategic tools and institute an educational forum allowing a wide coalition of healthcare and labor groups to engage with the NY City Council.
To get involved in New York, please contact Mandy Strenz at mandy@pnhpnymetro.org.

North Carolina
In North Carolina, members of Health Care for All-NC wrote and distributed a Medicare-for-All Voter Guide designed to inform the state’s residents about whether candidates supported a universal single-payer health system. The information in this nonpartisan guide was gathered using a candidate questionnaire compiled by Dr. Jonathan Kotch, Jonathan Michels, and SNaHP member Emma Tayloe. By compelling representatives to take a stand on the issue and keeping voters informed, chapter members helped to advance the cause of single payer in the state.
To get involved in Health Care for All-NC, please contact Jonathan Michels at jonscottmichels@gmail.com.
In Asheville, members of Health Care for All Western North Carolina (HCFA-WNC) threw a postcard party, mailing out over 100 postcards to help get out the vote in the area. The chapter also presented on “Why M4A” now to the retirement community of Givens Estates, and showed the PNHP video on ACO REACH to OLLI, an educational program series for retired citizens in the area. Members also participated in a Holiday Parade for Peace along with the Only One Earth Coalition.
To get involved in HCFA-WNC, please contact Terry Hash at theresamhash@gmail.com.

Health Care Justice NC in Charlotte has been gathering contact information and emailing legislative aides of all HR 1976 cosponsors, as well as Democratic members of the Energy & Commerce and Ways & Means Committees, to encourage them not to sign the annual letter circulated by the health insurance lobby expressing support of Medicare Advantage. The chapter also raised money that allowed five student leaders to attend the annual meeting in Boston last year. Finally, board member Zach Thomas composed, produced, and performed with other members in “Roll, Justice, Roll,” a new music video promoting Medicare for All with an emphasis on racial, gender, and other injustices.
To get involved in Health Care Justice NC, please contact Dr. George Bohmfalk at gbohmfalk@gmail.com.
West Virginia
One of PNHP’s newest chapters, in West Virginia, continues its activities around membership, education, and collaboration. Recruiting new members continues to be a top priority, with the chapter conducting phone outreach to state members and participating in the national membership renewal drive. A website is under development, and monthly meetings continue to be held featuring speakers from across the organization and beyond. Lawmakers in the state have not been receptive to visits or letters, so PNHP-WV has organized several protests at their offices to make their voices heard in ways that cannot be ignored. Finally, the chapter continues to collaborate on occasion with other groups working on health care reform, such as the WV Citizen Action Group and the WV Health Care for All Coalition.
To get involved in West Virginia, please contact Dr. Daniel Doyle doyledan348@gmail.com.
Wisconsin
The PNHP chapter in Wisconsin held a get together for medical students at Hoyt Park in Madison, which drew 30 attendees. There, members discussed issues related to medical education, research, patient access to care, and health care disparities. The chapter also hosted a booth at the Wisconsin LaborFest in Madison to promote Medicare for All. Finally, the chapter interviewed 3 candidates for the Wisconsin Senate race to ascertain their views on health care and promote PNHP’s vision of Medicare for All to them.
To get involved in Wisconsin, please contact Dr. Timothy Shaw at wisconsin.pnhp@gmail.com.

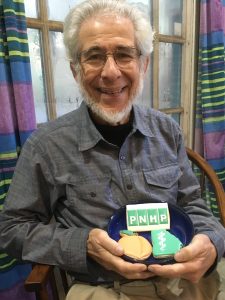
Protect Medicare Photo Petition
Medicare advocates have stood up by the thousands to demand the Biden administration end the REACH program—a transparent attempt to privatize Traditional Medicare that threatens the future of public health care in the U.S.
Nearly 20,000 have signed our online petition, and many have also submitting photo petitions. To submit your own photo petition, print this sign, take a selfie with it, and email your photo to lori@pnhp.org.

PNHP has posted more than 200 #StopREACH photo petitions to our social media channels, demonstrating widespread support for ending the program. Please share the following threads on your personal accounts!
- #StopREACH Photo Petitions 1: Twitter | Facebook
- #StopREACH Photo Petitions 2: Twitter | Facebook
- #StopREACH Photo Petitions 3: Twitter | Facebook
- #StopREACH Photo Petitions 4: Twitter | Facebook
- #StopREACH Photo Petitions 5: Twitter | Facebook
- #StopREACH Photo Petitions 6: Twitter | Facebook
- #StopREACH Photo Petitions 7: Twitter | Facebook
- #StopREACH Photo Petitions 8: Twitter | Facebook
- #StopREACH Photo Petitions 9: Twitter | Facebook
PNHP in the News
News items quoting PNHP members
- “Measure 111 asks Oregon voters to decide if healthcare should be a fundamental right,” KLCC, 10/17/22, featuring Dr. Samuel Metz
- “Many Insured Americans Are an Injury Away From Bankruptcy: Study,” HealthDay, 11/15/22, featuring Dr. Stephen Kemble
- “AARP Is Welcoming the Privatization of Medicare,” Jacobin, 11/22/22, featuring Dr. Susan Rogers
- “North Texas Home to Two of the Greediest Stories in Healthcare,” D Magazine, 1/13/23, featuring Dr. Susan Rogers
- “American Exceptionalism in One Heartbreaking, Grotesque Tweet,” Common Dreams, 1/25/23, featuring Dr. Adam Gaffney
- “Board Considers Alternatives to Statewide Gas Tax, Signs Letter of Support for Senior Living Community in McKinleyville and More,” Lost Coast Outpost, 2/1/23, featuring Patty Harvey and Dr. Corinne Frugoni
- “Students push single-payer health care system resolution,” Creightonian, 2/26/23, featuring India Claflin
Op-eds by PNHP members
- “What’s Wrong with Medicare Advantage?” by Dr. Stephen Kemble, Indypendent, 10/6/22
- “Be Careful and Do Some Research Before You Sign Up for ‘Medicare Advantage’,” by Patty Harvey and Dr. Corinne Frugoni, Lost Coast Outpost, 10/13/22
- “Medicare for All can put Georgia hospitals on solid financial footing,” by Jack Bernard, Atlanta Journal-Constitution, 10/14/22
- “Medicare Advantage? Medicare Disadvantage would be a better name.” by Dr. Jessica Schorr Saxe, The Charlotte Observer, 10/25/22
- “Commentary: Our health care system kills 168 people a day,” by Dr. Jay Brock, Fredericksburg Free Lance Star, 10/29/22
- “As I See It: Understanding Medicare Advantage,” by Dr. Bruce Thomson, Albany Democrat-Herald, 10/13/22
- “Enrolling in Medicare? What you should know about TV time, fraud and what’s next,” by Dr. Robert Stone, The Herald-Times, 11/17/22
- “Medicare Advantage’s plan is no such thing,” by Dr. Jay Brock, Fredericksburg Free Lance Star, 11/25/22
- “Medicare Advantage or taking advantage? Deadline for enrollment nears.” by Dr. Edward Chory, Lancaster Online, 11/27/22
- “Plenty of benefits of single-payer healthcare,” by Winchell Dillenbeck, Eureka Times Standard, 12/2/22
- “Milennials can save Medicare,” by Alexa D’Angelo, New York Daily News, 12/2/22
- “New to Medicare? Please consider this,” by Dr. Emily Kane, Juneau Empire, 12/3/22
- “Is it Medicare Advantage or Medicare Disadvantage?” by Jack Bernard, Charleston Gazette-Mail, 12/5/22
- “Traditional Medicare is under attack,” by Dr. Jack Mayer, Vermont Digger, 12/14/22
- “Big Pharma spent more on Stock buybacks and Dividends than on Research and Development even during COVID,” by F. Douglas Stephenson, Informed Comment, 1/8/23
- “Private entities are chiseling away at Medicare as we know it,” by Patty Harvey and Dr. Corinne Frugoni, Times Standard, 1/14/23
- “Is Medicare there for those who need it?” by Dr. Mary McDevitt, Sonoma County Gazette, 1/31/23
- “Democrats and Republicans agree: Cut the waste in Medicare Advantage,” by Diane Archer and Dr. Susan Rogers, The Hill, 2/9/23
- “How to address the unsustainably rising healthcare costs,” by Kenneth Dolkart, New Hampshire Business Review, 2/9/23
- “Privatizing Medicare is the wrong way to go,” by Joshua Freeman, Arizona Daily Star, 3/2/23
Letters to the editor by PNHP members
- “Direct Contracting Allows Companies to Control the Healthcare of Medicare and Medicare Supplement Beneficiaries,” by Mike Gatton, Connecticut Examiner, 9/28/22
- “Medicare Privatization,” by Mike Gatton, Arizona Daily Star, 10/1/22
- “Have you heard about Medicare Direct Contracting?” by Mike Gatton, Hudson Reporter, 10/10/22
- “How Private Insurers Exploit Medicare,” by Cheryl Kunis, The New York Times, 10/23/22
- “‘Advantage’ plans are eroding Medicare’s mission,” by Lloyd Alterman, New Jersey Star-Ledger, 10/23/22
- “Don’t fall for the Medicare ‘disadvantage’ scam,” by Richard Cook, Southern Maryland News, 10/31/22
- “Medicare changes incentivize less care,” by Pat Russo, Tribune Chronicle, 11/9/22
- “The disadvantaged of Medicare Advantage,” by Robert Kiefner, Concord Monitor, 11/9/22
- “Local Illinois vote suggests Medicare for All is popular,” by Pam Gronemeyer, St. Louis Post Dispatch, 11/14/22
- “Medicare Advantage may be a scam,” by Ellen Kaczmarek, Asheville Citizen Times, 11/16/22
- “Don’t be fooled by Medicare Advantage,” by Hal Chorny, Daily Freeman, 11/23/22
- “Between Medicare Advantage promotions,” by Pat Kanzler, RN, Times Standard, 11/25/22
- “Medicare (Dis)Advantage,” by Barbara Ross, News Tribune, 11/27/22
- “Medicare Advantage’s Big Disadvantage,” by Dwight Oxley, Wall Street Journal, 11/30/22
- “Scam tactics of Medicare Advantage plans should be covered in The Tribune,” by Christine Helfrich, Salt Lake Tribune, 12/4/22
- “A Better Hospital Model,” by Sarah K. Weinberg, The New York Times, 12/10/22
- “Health care: Profit-making sickness,” by Walter J. Alt, The Seattle Times, 1/4/23
- “Health care inequity,” by G. Richard Dundas, Times Argus, 1/19/23
- “Denying patients, rewarding physicians,” by Hal Chorny, Daily Freeman, 1/20/23
- “Health care should be available and affordable for all,” by G. Richard Dundas, Brattleboro Reformer, 1/24/23
- “Stop ACO REACH,” by Patty Harvey, Mad River Union, 1/24/23
- “Access to health care should be expanded, not restricted,” by Henry Kahn, Atlanta Journal-Constitution, 1/24/23
- “REACH could privatize Medicare,” by Doris Chorny, River Reporter, 2/9/23
- “Medicare Advantage is a bad deal for patients and taxpayers,” by Michael Hamant, Arizona Daily Star, 2/10/23
- “Don’t let Corporate America Take Over Medicare,” by Paul Cooper, Shawangunk Journal, 2/21/23
- “Our state needs a single payer system,” by Chris Van Hemelrijick, The Independent, 2/23/23
- “Liz Fowler on the Defensive (for now),” by Paul Cooper, Hudson Valley One, 3/1/23
