“How are you going to pay for it?” Single-payer skeptics often ask this question in a bad-faith attempt to discredit Medicare for All. But the answer is simple: We’re already spending enough on health care. We’re just not getting our money’s worth.
Interested in how single payer would affect your personal finances? Check out the Medicare for All household savings calculator, which was developed by a team of health policy experts including PNHP leaders Drs. James G. Kahn, Henry L. Abrons, and Rachel Madley.
PNHP-MN interns and medical students Conor Nath and Preethiya Sekar reviewed the evidence for overall health spending by analyzing a decade’s worth of post-ACA single-payer financing studies (John A. Nyman, Ph.D.; Gordon Mosser, M.D.; and Kenneth Englehart, M.D. served as advisors). The team developed detailed infographics for each study (see below) as well as a primer and a PowerPoint presentation that offer an overview of their project.
PNHP will add new financing studies to this page as they are published (most recent study appearing first). For archival links to pre-ACA analyses, state-based studies, and a succinct statement from former American Public Health Association president Dr. Linda Rae Murray, click here.
It’s also worth noting that several high-profile Medicare-for-All financing plans have been released by elected officials: one from Sen. Elizabeth Warren and one from Sen. Bernie Sanders. PNHP offered comment on these proposals, here.
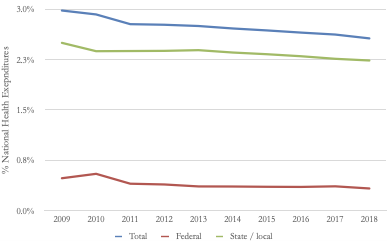
Of course, the status quo is unsustainable. National health spending continues to grow at a rapid clip, year after year, with the latest figures from 2022 showing a 4.1% increase from 2021, to $4.5 trillion. That’s more than enough to finance all medically necessary care for every U.S. resident while totally eliminating out-of-pocket spending.
Bottom line: a single-payer national health program is not only affordable, it’s the only affordable option.
“Economic Effects of Five Illustrative Single-Payer Health Care Systems”
Congressional Budget Office 2022
learn more“How CBO Analyzes the Costs of Proposals for Single-Payer Health Care Systems That Are Based on Medicare’s Fee-for-Service Program”
Congressional Budget Office 2020
learn more“Improving the Prognosis of Health Care in the USA”
Yale School of Public Health 2020
learn more“Projected costs of single-payer healthcare financing in the United States: A systematic review of economic analyses”
PLOS Medicine 2020
learn more“From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare on Coverage and Costs”
The Urban Institute 2019
learn more“Yes, We Can Have Improved Medicare for All”
Hopbrook Institute 2019
learn more“National Health Spending Estimates Under Medicare for All”
RAND 2019
learn more“Economic Analysis of Medicare for All”
Political Economy Research Institute (PERI) 2018
learn more“The Costs of a National Single-Payer Healthcare System”
Mercatus Center 2018
learn more“The Sanders Single-Payer Health Care Plan: The Effect on National Health Expenditures and Federal and Private Spending”
The Urban Institute 2016
learn more“An Analysis of Senator Sanders’ Single-Payer Plan”
Emory University 2016
learn more“Exploring Single-Payer Alternatives for Health Care Reform”
RAND 2016
learn more“Funding HR 676: The Expanded and Improved Medicare for All Act”
University of Massachusetts at Amherst 2013
learn more“Economic Effects of Five Illustrative Single-Payer Health Care Systems”
Congressional Budget Office 2022
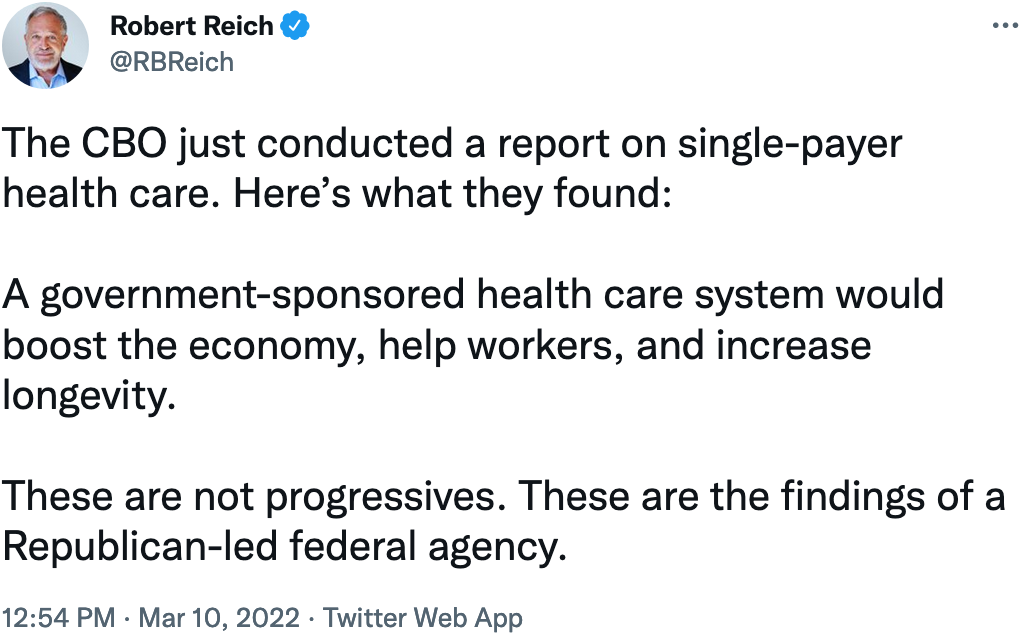
Title: Economic Effects of Five Illustrative Single-Payer Health Care Systems
Year: 2022
Authors: Jaeger Nelson
Institution: Congressional Budget Office
Plan Analyzed: “Five illustrative options” for a single-payer national health program, not strictly based on existing legislation
Percent Change in National Health Expenditure under M4A: Ranging from a decrease of $743 billion to an increase of $290 billion in 2030
Read Study:
Economic Effects of Five Illustrative Single-Payer Health Care Systems, Working Paper
Abstract:
Further Reading:
- Health Justice Monitor entry by Drs. Don McCanne and Jim Kahn
- “The Government’s Own Number Crunchers Agree: We Need Medicare for All” by David Sirota and Aditi Ramaswami, Jacobin, Feb. 25, 2022
“How CBO Analyzes the Costs of Proposals for Single-Payer Health Care Systems That Are Based on Medicare’s Fee-for-Service Program”
Congressional Budget Office 2020
Title: How CBO Analyzes the Costs of Proposals for Single-Payer Health Care Systems That Are Based on Medicare’s Fee-for-Service Program
Year: 2020
Authors: CBO’s Single-Payer Health Care Systems Team
Institution: Congressional Budget Office
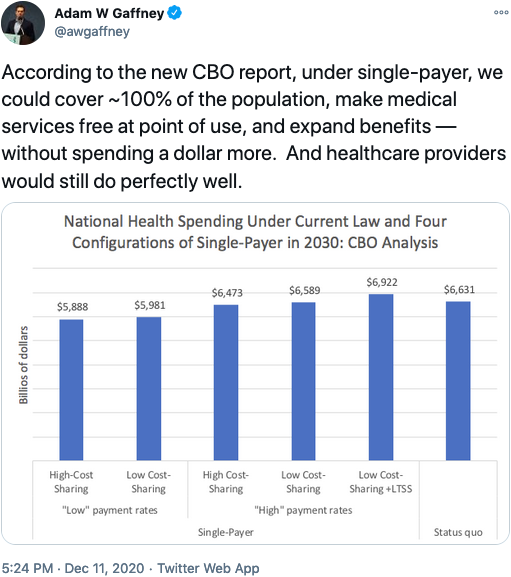
Plan Analyzed: “Five illustrative options” for a single-payer national health program, not based on H.R. 1384 or S.1129
Percent Change in National Health Expenditure under M4A (10-year): Ranging from a decrease of $0.7 trillion to an increase of $0.3 trillion in 2030
Read Study:
Summary:
Further Reading:
- Blog by CBO Director Phillip Swagel
- Quote of the Day by Dr. Don McCanne
- “CBO: Medicare for All Reduces Health Spending” by Matt Bruenig, People’s Policy Project
- “Utilization of health care services after large coverage expansions” series of studies debunking the claim the health care utilization would spike under single payer
- “Key Design Components and Considerations for Establishing a Single-Payer Health Care System” published by the Congressional Budget Office, May 2019
Congressional Hearings on 2019 Report:
back to top“Improving the Prognosis of Health Care in the USA”
Yale School of Public Health 2020
Title: Improving the prognosis of health care in the USA
Year: 2020
Authors: Alison P. Galvani, Alyssa S. Parpia, Eric M. Foster, Burton H. Singer, Meagan C. Fitzpatrick
Institution: Yale School of Public Health
Funding Source: N/A
Plan Analyzed: S. 1804 Medicare for All Act of 2017
Percent Change in National Health Expenditure under M4A (1-year): -13.1% (2017)
Percent Change in National Health Expenditure under M4A (10-year): NS
Increase in Federal health expenditures: $773 billion (2017)
Read Study:
Improving the prognosis of health care in the USA
Study Abstract:
Although health care expenditure per capita is higher in the USA than in any other country, more than 37 million Americans do not have health insurance, and 41 million more have inadequate access to care. Efforts are ongoing to repeal the Affordable Care Act which would exacerbate health care inequities. By contrast, a universal system, such as that proposed in the Medicare for All Act, has the potential to transform the availability and efficiency of American health care services. Taking into account both the costs of coverage expansion, and the savings that would be achieved through the Medicare for All Act, we calculate that a single-payer, universal health care system is likely to lead to a 13% savings in national health-care expenditure, equivalent to more than US$450 billion annually (based on the value of the US$ in 2017). The entire system could be funded with less financial outlay than is incurred by employers and households paying for health care premiums combined with existing government allocations. This shift to single-payer health care would provide the greatest relief to lower-income households. Furthermore, we estimate that ensuring health care access for all Americans would save more than 68,000 lives and 1.73 million life-years every year compared with the status quo.
Overview:
- In early 2020, Alison Galvani published a cost-analysis of the Senate Medicare for All bill, S. 1804. Of note, Galvani served as an “informal unpaid adviser” to the writers of this particular bill.
- The Yale study focuses on:
- Savings from reduced fees for hospital and clinical services, unified system for billing and administration, pharmaceutical price negotiation
- The cost of expansion of coverage and services
- Financing plan effects on employers and households
- Public health approach to estimate “life-years” saved by Medicare for All
- Positive spillovers from emphasizing preventive services
- Creation of a Tool that can model costs/savings as well as revenue generation
Further Reading:
SHIFT Tool allowing users to modify inputs and assumptions
back to top“Projected costs of single-payer healthcare financing in the United States: A systematic review of economic analyses”
PLOS Medicine 2020
Title: Projected costs of single-payer healthcare financing in the United States: A systematic review of economic analyses
Year: 2020
Author: Christopher Cai, Jackson Runte, Isabel Ostrer, Kacey Berry, Ninez Ponce, Michael Rodriguez, Stefano Bertozzi, Justin S. White, James G. Kahn
Institution: University of California, San Francisco
Plan Analyzed: Economic analyses of 22 single-payer plans published over the past 30 years
Percent Change in National Health Expenditure under M4A: -3.46% (median savings for the 19 of 22 analyses that predicted net savings)
Read Study:
Study Abstract:
Background: The United States is the only high-income nation without universal, government-funded or -mandated health insurance employing a unified payment system. The US multi-payer system leaves residents uninsured or underinsured, despite overall healthcare costs far above other nations. Single-payer (often referred to as Medicare for All), a proposed policy solution since 1990, is receiving renewed press attention and popular support. Our review seeks to assess the projected cost impact of a single-payer approach.
Methods and findings: We conducted our literature search between June 1 and December 31, 2018, without start date restriction for included studies. We surveyed an expert panel and searched PubMed, Google, Google Scholar, and preexisting lists for formal economic studies of the projected costs of single-payer plans for the US or for individual states. Reviewer pairs extracted data on methods and findings using a template. We quantified changes in total costs standardized to percentage of contemporaneous healthcare spending. Additionally, we quantified cost changes by subtype, such as costs due to increased healthcare utilization and savings due to simplified payment administration, lower drug costs, and other factors. We further examined how modeling assumptions affected results. Our search yielded economic analyses of the cost of 22 single-payer plans over the past 30 years. Exclusions were due to inadequate technical data or assuming a substantial ongoing role for private insurers. We found that 19 (86%) of the analyses predicted net savings (median net result was a savings of 3.46% of total costs) in the first year of program operation and 20 (91%) predicted savings over several years; anticipated growth rates would result in long-term net savings for all plans. The largest source of savings was simplified payment administration (median 8.8%), and the best predictors of net savings were the magnitude of utilization increase, and savings on administration and drug costs (R2 of 0.035, 0.43, and 0.62, respectively). Only drug cost savings remained significant in multivariate analysis. Included studies were heterogeneous in methods, which precluded us from conducting a formal meta-analysis.
Conclusions: In this systematic review, we found a high degree of analytic consensus for the fiscal feasibility of a single-payer approach in the US. Actual costs will depend on plan features and implementation. Future research should refine estimates of the effects of coverage expansion on utilization, evaluate provider administrative costs in varied existing single-payer systems, analyze implementation options, and evaluate US-based single-payer programs, as available.
Further reading:
back to top“From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare on Coverage and Costs”
The Urban Institute 2019
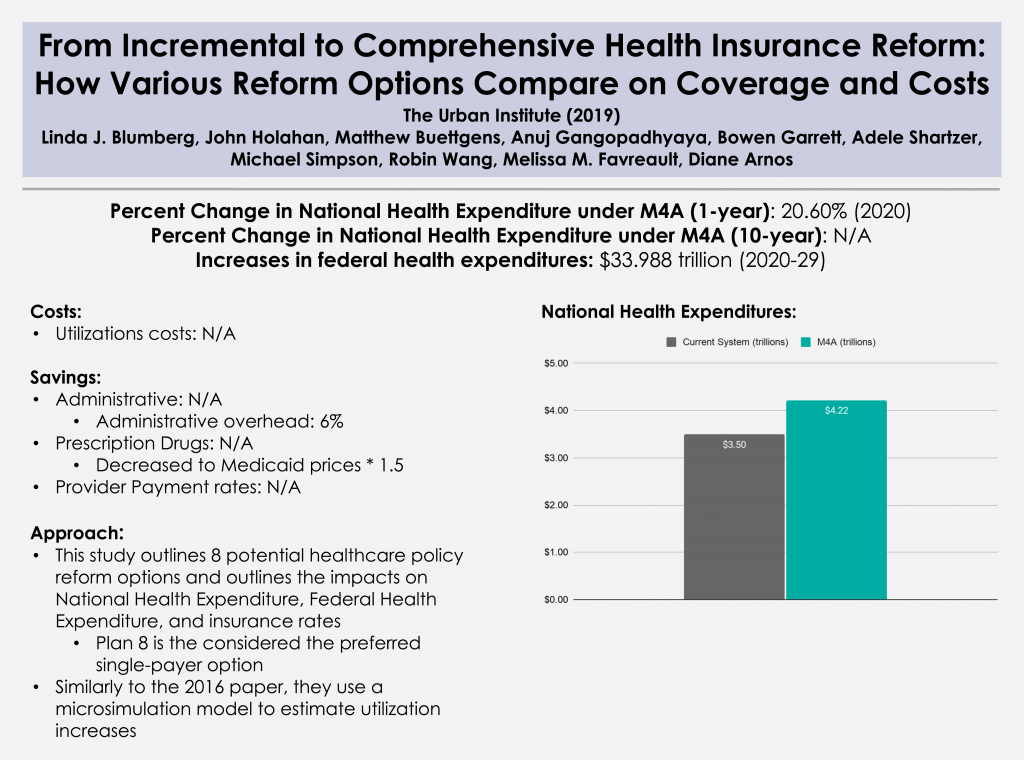
Title: From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare on Coverage and Costs
Year: 2019
Author: Linda J. Blumberg, John Holahan, Matthew Buettgens, Anuj Gangopadhyaya, Bowen Garrett, Adele Shartzer, Michael Simpson, Robin Wang, Melissa M. Favreault, and Diane Arnos
Institution: Urban Institute
Funding Source: The Commonwealth Fund
Plan Analyzed: “Reform 8”
Percent Change in National Health Expenditure under M4A (1-year): 20.6% (2020)
Percent Change in National Health Expenditure under M4A (10-year): NS
Increases in federal health expenditures: $33.988 trillion (2020-29)
Read Study:
Abstract:
Policymakers, including candidates in the 2020 presidential campaign and members of Congress, have proposed a variety of options to address the shortcomings of the current health care system. These range from improvements to the Affordable Care Act to robust single-payer reform.
There are numerous challenging trade-offs when choosing an approach to health care reform, including covering the uninsured, improving the affordability of health care, and raising the government funding required to implement them. The public and policymakers alike need more information about the potential effects of various health reform proposals.
This study, funded by the Commonwealth Fund, analyzes eight health care reforms and their potential effects on health insurance coverage and spending. Each of the analyzed reform proposals makes health insurance considerably more affordable by reducing people’s premiums and cost sharing. Some reforms also reduce US health care costs, and all require additional federal dollars.
Overview:
- This study is unique in that it outlines 8 potential health care policy reform options, and then outlines impacts on national health expenditures, federal health expenditure, and insurance rates. It utilizes the same microsimulation approach that the Urban institute utilized in its 2016 paper.
- Reforms considered by this paper include those that:
- Build on the ACA
- Reform 1: Enhanced financial assistance
- Reform 2: Federal individual mandate and STLD prohibitions
- Reform 3: Filling the Medicaid eligibility gap
- Reform 4: Public option and/or capped provider payment rates
- Reform 5: CARE, no ESI firewall
- Reform 6: Further enhanced financial assistance
- Replace the ACA
- Reform 7: Single-payer lite
- Reform 8: Single-payer enhanced
- Build on the ACA
PNHP Response:
PNHP co-founders Drs. David Himmelstein and Steffie Woolhandler found that “the Urban Institute analysis grossly underestimates the administrative savings under single payer, and projects increases in the number of doctor visits and hospitalizations that far exceed the capacity of doctors and hospitals to provide this added care.” Their full critique here, and a QOTD response from Dr. Don McCanne, including comments from PNHP president Dr. Adam Gaffney, here.
Further Reading:
Comparing Health Insurance Reform Options: From “Building on the ACA” to Single Payer
back to top“Yes, We Can Have Improved Medicare for All”
Hopbrook Institute 2019
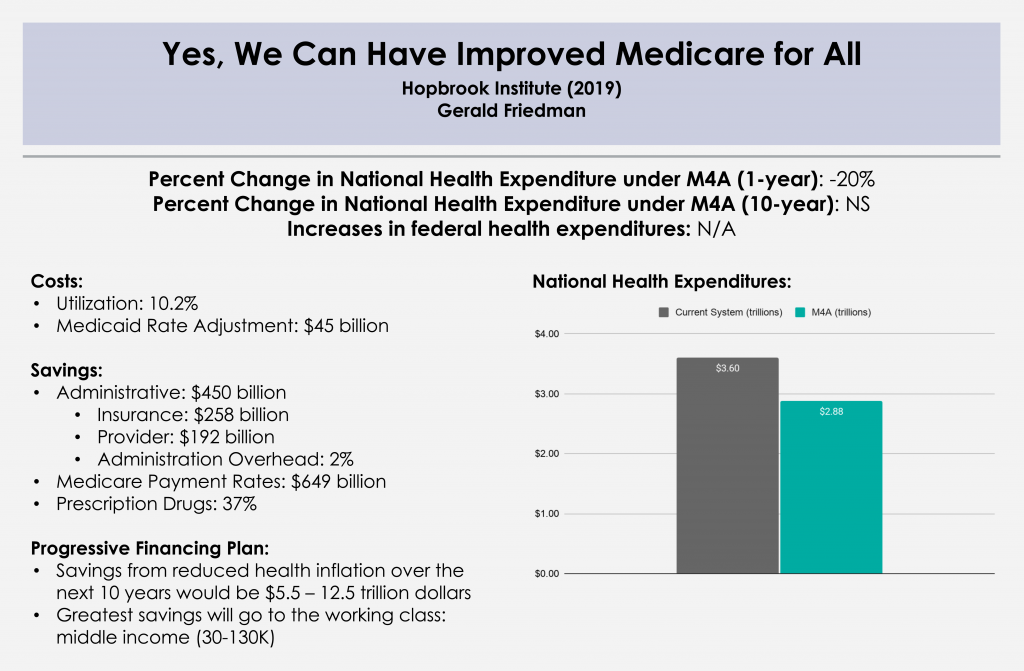
Title: Yes, We Can Have Improved Medicare for All
Year: 2019
Author: Gerald Friedman
Institution: University of Massachusetts at Amherst
Funding Source: Hopbrook Institute
Plan Analyzed: H.R. 676
Percent Change in National Health Expenditure under M4A (1-year): -20.0% (2019)
Percent Change in National Health Expenditure under M4A (10-year): -20.6% (2019-28)
Read Study:
Yes, We Can Have Improved Medicare for All
Abstract:
Growing public support for universal health coverage through a public program has provoked increasing attention to the question of how to finance such a program. There should not be any controversy about our ability to pay for universal health care. Given the nearly universal agreement that the current health-care system involves administrative waste and monopoly pricing, a system that would be more efficient and would reduce both should certainly be affordable. Studies finding higher costs for universal coverage programs have reached their conclusions by acknowledging efficiency savings but dismissing them by emphasizing, even exaggerating, the higher costs of providing better access to health care. Such studies provide a poor guide to the possibilities for an overhaul of our health-care finance system. In this paper, I discuss the financing of a universal health-care program, beginning with a discussion of current projected spending and the savings to be achieved through administrative efficiency and reducing monopoly pricing. Next, I outline increased spending associated with universal coverage through covering the uninsured and reducing barriers to access. I consider the net cost of universal coverage, after taking account of savings and the cost of extending and improving coverage, under various scenarios with alternative immediate savings and savings over time. Finally, I discuss sources of funding for such a program, beginning with public funds already committed and including possible additional sources of revenue. I develop funding plans under a variety of assumptions regarding the course of the single-payer system, and under alternative assumptions regarding revenue sources. This work shows that compared with the current system of health-care finance, a program of Improved Medicare for All could save Americans over $1 trillion in the first year, and savings could increase over time. Because some of the savings would be returned to health care through programs of universal coverage and improved access, net savings could be over $700 billion in the first year, rising over the next decade. Depending on the assumptions made and the program details, total financial savings, after taking account of program improvements, would come to $10 trillion or more over the next decade, on top of gains in quality of life and reduced mortality through universal access. A variety of models are compared, with varying assumptions of the magnitude of administrative savings and savings through reduced monopoly rents, as well as savings from bending the cost curve and maintaining some cost-sharing. Overall, the ten-year national savings on health-care expenditures range from a low of over $6 trillion to a high of over $13 trillion. In every model tested, Improved Medicare for All is cheaper than the current system even while providing improved health care.
Overview:
Comprehensive cost analysis conducted by Gerald Friedman updating his previous work on the subject with similar considerations for financing options.
- Section 1: Current spending and waste
- Administrative savings in provider offices
- Savings from pricing at Medicare negotiated rates
- Drugs and medical devices
- Hospital and physician practices
- Section 2: Additional spending with universal coverage
- Medicare premiums
- Cost of universal coverage
- Cost of eliminating barriers to access
- Section 3: Total Spending with Medicare for All
- Section 4: Paying for Medicare for All
- Available revenues
- New revenues
- Conclusion: We can afford Improved Medicare for All
“National Health Spending Estimates Under Medicare for All”
RAND 2019
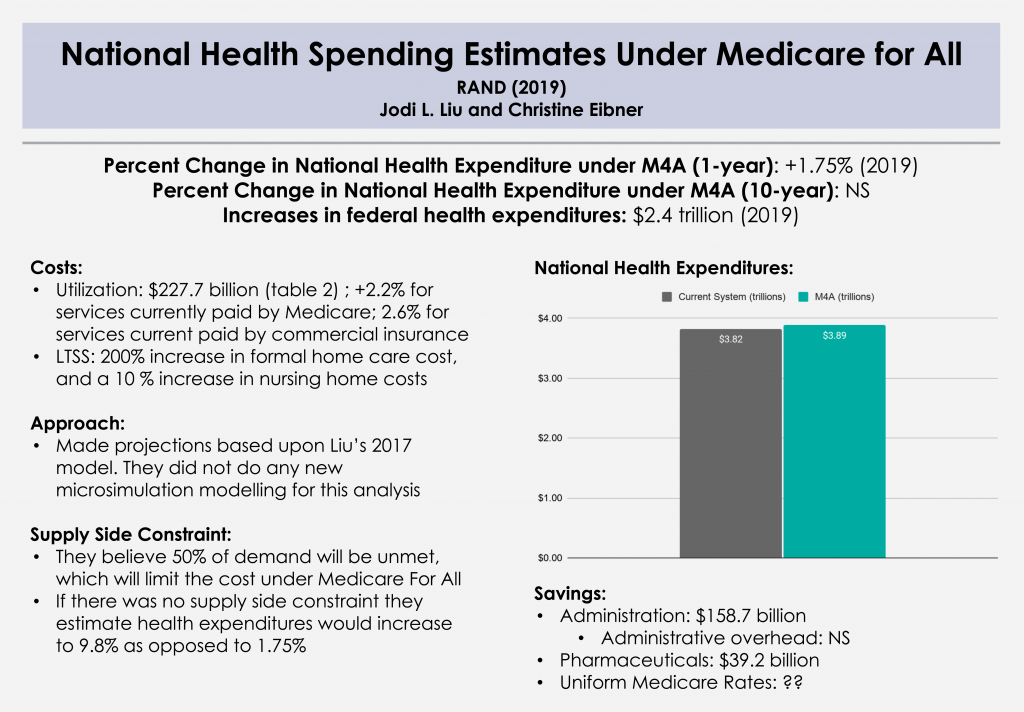
Title: National Health Spending Estimates Under Medicare for All
Year: 2019
Authors: Jodi L. Liu and Christine Eibner
Institution: RAND
Funding Source: Modeled after H.R. 1384
Plan Analyzed: S. 1782 / H.R. 1200
Percent Change in National Health Expenditure under M4A (1-year): +1.75% (2019)
Percent Change in National Health Expenditure under M4A (10-year): NS
Increases in federal health expenditures: $2.4 trillion (2019)
Read Study:
National Health Spending Estimates Under Medicare for All
Study Abstract:
We estimate that total health expenditures under a Medicare-for-All plan that provides comprehensive coverage and long-term care benefits would be $3.89 trillion in 2019 (assuming such a plan was in place for all of the year), or a 1.8 percent increase relative to expenditures under current law. This estimate accounts for a variety of factors including increased demand for health services, changes in payment and prices, and lower administrative costs. We also include a supply constraint that results in unmet demand equal to 50 percent of the new demand. If there were no supply constraint, we estimate that total health expenditures would increase by 9.8 percent to $4.20 trillion.
While the 1.8 percent increase is a relatively small change in national spending, the federal government’s health care spending would increase substantially, rising from $1.09 trillion to $3.50 trillion, an increase of 221 percent.
Overview:
- An update done by extrapolating projections from the microsimulation modelling in the 2016 RAND study. No new modelling was undertaken for this analysis.
- This study considers:
- Increased demand for medical services and long-term care services and supports (LTSS)
- Savings from all-payer rates for services, prices for drugs and devices, administrative costs
- Supply-side constraints for services
- Level of financing needed for Medicare For All
PNHP Response:
Regarding increased utilization, we would highlight three studies from 2019 that found large-scale coverage expansions in the United States (Medicare/Medicaid in the late 1960s and the ACA in the early 2010s) did not lead to a society-wide increase in hospitalizations or doctor visits, and that large-scale expansions in other nations also did not cause a spike in utilization. (See “Utilization of health care services after large coverage expansions.”)
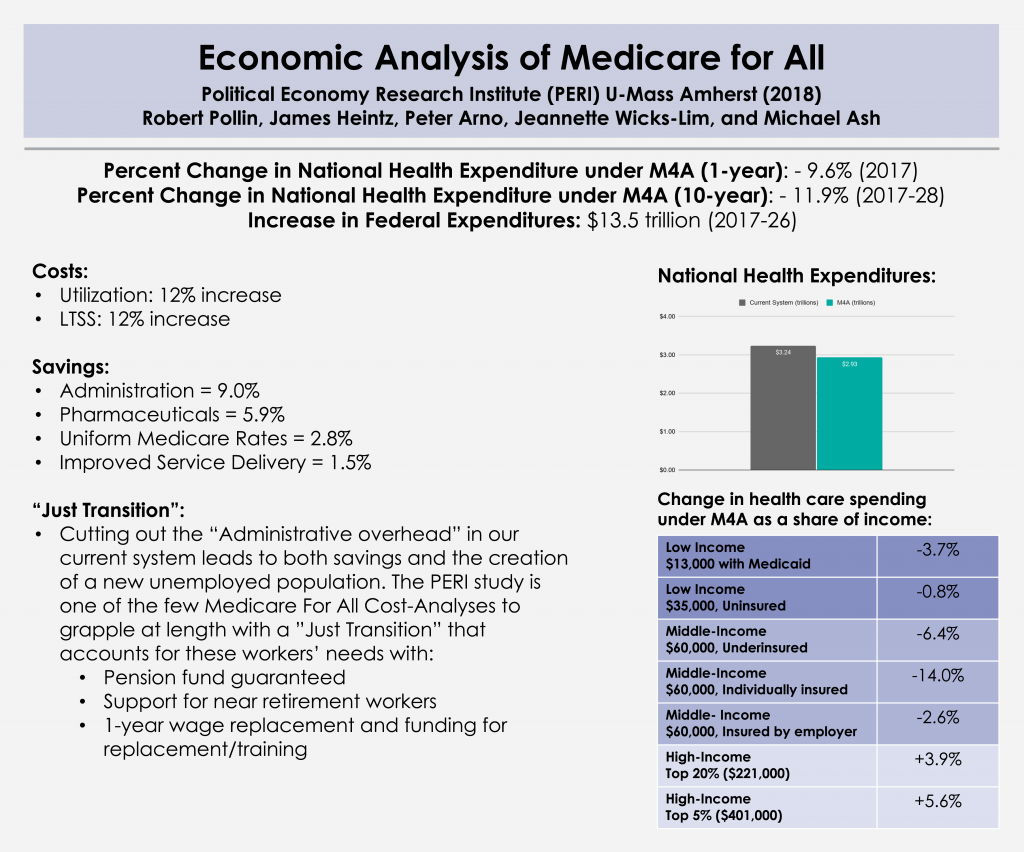
back to top“Economic Analysis of Medicare for All”
Political Economy Research Institute (PERI) 2018
Title: Economic Analysis of Medicare for All
Year: 2018
Author: Robert Pollin, James Heintz, Peter Arno, Jeannette Wicks-Lim, and Michael Ash
Institution: Political Economy Research Institute (PERI) U-Mass Amherst
Funding Source: California Nurses Association/National Nurses United
Plan Analyzed: S. 1804 Medicare for All Act of 2017
Percent Change in National Health Expenditure under M4A (1-year): -9.6% (2017)
Percent Change in National Health Expenditure under M4A (10-year): -11.9% (2017-26)
Increase in Federal health expenditures: $1.35 trillion (2017-26)
Read Study:
PERI – Economic Analysis of Medicare for All
Study Abstract:
This study by PERI researchers Robert Pollin, James Heintz, Peter Arno, Jeannette Wicks-Lim and Michael Ash presents a comprehensive analysis of the prospects for a Medicare-for-All health care system in the United States. The most fundamental goals of Medicare for All are to significantly improve health care outcomes for everyone living in the United States while also establishing effective cost controls throughout the health care system. These two purposes are both achievable. As of 2017, the U.S. was spending about $3.24 trillion on personal health care—about 17 percent of total U.S. GDP. Meanwhile, 9 percent of U.S. residents had no insurance and 26 percent were underinsured—they were unable to access needed care because of prohibitively high costs. Other high-income countries spend an average of about 40 percent less per person and produce better health outcomes. Medicare for All could reduce total health care spending in the U.S. by nearly 10 percent, to $2.93 trillion, while creating stable access to good care for all U.S. residents.
Overview:
- The PERI study is a lengthy and comprehensive cost-analysis study. The authors explain their assumptions and counterfactuals at length and show their calculations in a very easy-to-follow format.
- The Report contains 7 sections:
- Chapter 1: Underscores why affordable health care can improve health outcomes
- Chapters 2-3: Identifies sources of costs and savings
- Chapter 4: Financing Plans for Medicare For All
- Chapter 5: Effects of financing plans on families (based on income) and businesses (small, medium, and large)
- Chapter 6: Considers the logistics and the costs of transitioning from our current system to a single-payer system (“Just Transition”)
- Chapter 7: Estimates the effects of Medicare for All on health care spending as a share of US GDP, and other macroeconomic impacts
PNHP Response:
PNHP co-founders Drs. Steffie Woolhandler and David Himmelstein, and PNHP president Dr. Adam Gaffney, submitted a reviewer assessment of the PERI study. They note that the PERI analysis may understate administrative savings, but overall find it to be a “highly credible economic analysis.”
Further Reading:
Facing job loss with Just Transition (KHN)
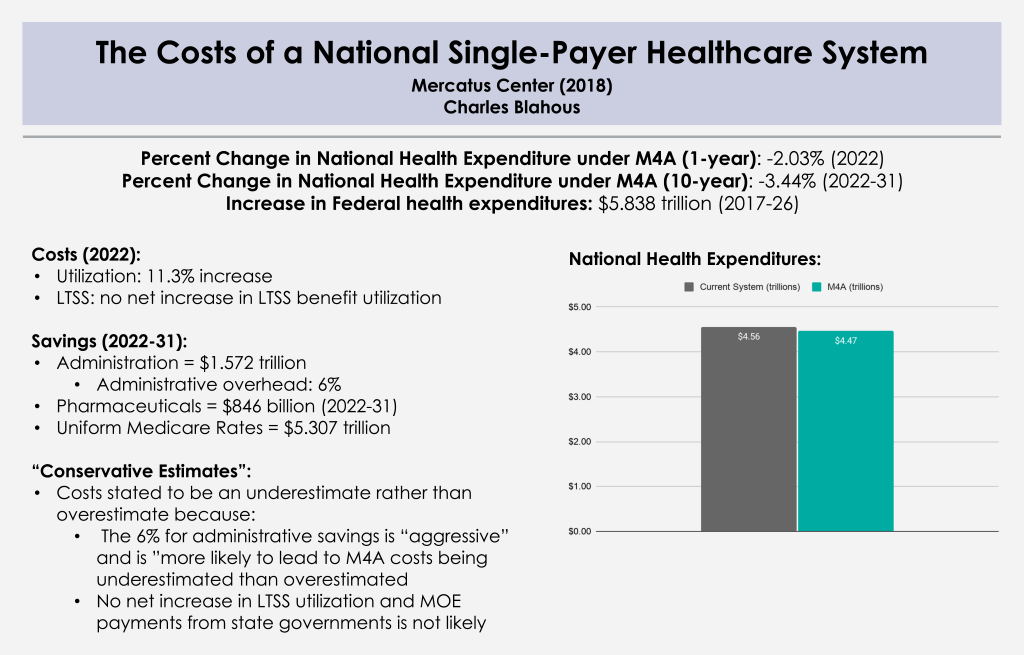
back to top“The Costs of a National Single-Payer Healthcare System”
Mercatus Center 2018
Title: The Costs of a National Single-Payer Healthcare System
Year: 2018
Authors: Charles Blahaus
Institution: Mercatus Center
Funding Source: Koch
Plan Analyzed: S. 1804 Medicare for All Act of 2017
Percent Change in National Health Expenditure under M4A (1-year): -2.03% (2022)
Percent Change in National Health Expenditure under M4A (10-year): -3.44% (2022-31)
Increase in Federal health expenditures: $5.838 trillion (2017-26)
Read Study:
The Costs of a National Single-Payer Healthcare System
Study Abstract:
The leading current bill to establish single-payer health insurance, the Medicare for All Act (M4A), would, under conservative estimates, increase federal budget commitments by approximately $32.6 trillion during its first 10 years of full implementation (2022–2031), assuming enactment in 2018. This projected increase in federal health care commitments would equal approximately 10.7 percent of GDP in 2022, rising to nearly 12.7 percent of GDP in 2031 and further thereafter. Doubling all currently projected federal individual and corporate income tax collections would be insufficient to finance the added federal costs of the plan. It is likely that the actual cost of M4A would be substantially greater than these estimates, which assume significant administrative and drug cost savings under the plan, and also assume that health care providers operating under M4A will be reimbursed at rates more than 40 percent lower than those currently paid by private health insurance.
Overview:
- The Mercatus Report focuses on national health expenditures (NHE), but places particular emphasis on federal health expenditures.
- The Report focuses on:
- An overview of the findings and rationale for why Blahaus believes his estimate is an “underestimate”
- Detail Increased Demand and Utilization assumptions and Long Term Services and Supports (LTSS)
- Savings from Provider Payment Reductions, Drug Costs, Administrative Savings. Blahaus underscores that all of these savings will likely not be achieved because his estimates require a perfect transition from policy to practice. (Administrative Tasks, Prescription Drug Negotiation, etc) operate their optimal capacity/efficiency
- Effects on NHE and the Federal Budget, expressing skepticism about financing plans despite not laying out any particular financing plans
- Appendix with Financial Effects of different scenarios under Medicare for All
PNHP Response:
PNHP co-founders Drs. David Himmelstein and Steffie Woolhandler critique the Mercatus reports as “ideology masquerading as health economics.”
Further Reading:
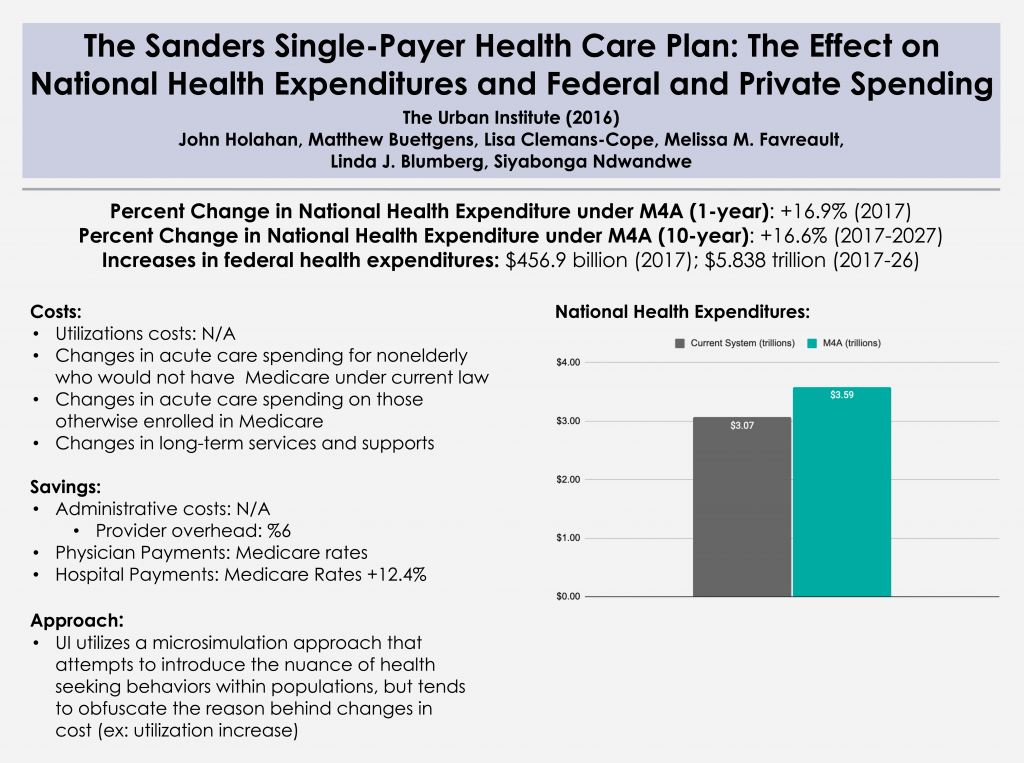
back to top“The Sanders Single-Payer Health Care Plan: The Effect on National Health Expenditures and Federal and Private Spending”
The Urban Institute 2016
Title: The Sanders Single-Payer Health Care Plan: The Effect on National Health Expenditures and Federal and Private Spending
Year: 2016
Author: John Holahan, Lisa Clemans-Cope, Matthew Buettgens, Melissa Favreault, Linda J. Blumberg, and Siyabonga Ndwandwe
Institution: Urban Institute
Funding Source: N/A
Plan Analyzed: Bernie Sanders’ 2016 campaign proposal (eventually became S. 1804 Medicare for All Act of 2017)
Percent Change in National Health Expenditure under M4A (1-year): 16.9% (2017)
Percent Change in National Health Expenditure under M4A (10-year): 16.6% (2017-26)
Increases in federal health expenditures: $456.9 billion (2017)
Read Study:
The Sanders Single-Payer Health Care Plan
Abstract:
Presidential candidate Bernie Sanders proposed a single-payer system to replace all current health coverage. His system would cover all medically necessary care, including long-term care, without cost-sharing. We estimate that the approach would decrease the uninsured by 28.3 million people in 2017. National health expenditures would increase by $6.6 trillion between 2017 and 2026, while federal expenditures would increase by $32.0 trillion over that period. Sanders’s revenue proposals, intended to finance all health and nonhealth spending he proposed, would raise $15.3 trillion from 2017 to 2026—thus, the proposed taxes are much too low to fully finance his health plan.
Overview:
- 2016 study done by the Urban Institute utilizing a microsimulation approach to conduct a cost analysis of the Sanders Medicare for All proposal from the 2016 presidential primary in contrast to projection studies that had been done up to that point.
- This study considers how cost would be affected by:
- Acute healthcare spending increases by non-elderly individuals who would not otherwise be enrolled in Medicare
- Acute healthcare spending increases by those who would otherwise be enrolled in medicare under currently law
- Increase in utilization costs for long term services and supports
- This study discusses
- Assumptions that tend to over/underestimate costs when considering M4A.
Further Reading:
- PNHP Response
- Urban Institute Response to PNHP
- PNHP Counter-Response
- Gordon Mosser Critical Review and comment by Dr. Don McCanne
“An Analysis of Senator Sanders’ Single-Payer Plan”
Emory University 2016
Title: An Analysis of Senator Sanders Single Payer Plan
Year: 2019
Author: Kenneth Thorpe
Institution: Emory University
Plan Analyzed: S. 1129
Increases in federal health expenditures: $1.9 trillion (2017) and $24.6 trillion (2017-26)
Read Study:
An Analysis of Senator Sanders’s Single Payer Plan
Abstract:
Senator Sanders has proposed eliminating private health insurance and the exchanges created through the Affordable Care Act and replacing it with a universal Medicare program with no cost sharing. The plan would shift virtually all health care spending from private and public sources today onto the federal budget. The campaign estimates his plan would cost an average of $1.38 trillion per year over the next decade. They outline a variety of payroll and income tax increases, higher taxes for capital gains and dividends, taxes on estates of high income households and eliminate tax breaks that subsidize health insurance. Collectively he claims these taxes fully pay for the costs of the single payer plan. The analysis presented below however estimates that the average annual cost of the plan would be approximately $2.5 trillion per year creating an average of over a $1 trillion per year financing shortfall. To fund the program, payroll and income taxes would have to increase from a combined 8.4 percent in the Sanders plan to 20 percent while also retaining all remaining tax increases on capital gains, increased marginal tax rates, the estate tax and eliminating tax expenditures. The plan would create enormous winners and losers even with the more generous benefits with respect to what households and businesses pay today compared to what they would pay under a single payer plan. Overall, over 70 percent of working privately insured households would pay more under a fully funded single payer plan than they do for health insurance today.
Overview:
This study is unique because it primarily focuses on the increase in federal health care spending and how this increase might be financed.
This study considers:
- The impact of increased payment rates for current Medicare/Medicaid beneficiaries.
- Financing mechanisms for increased federal spending.
- Populations that would be “at-risk” based on proposed financing mechanisms.
Further Reading:
Gordon Mosser Critical Review and comment by Dr. Don McCanne
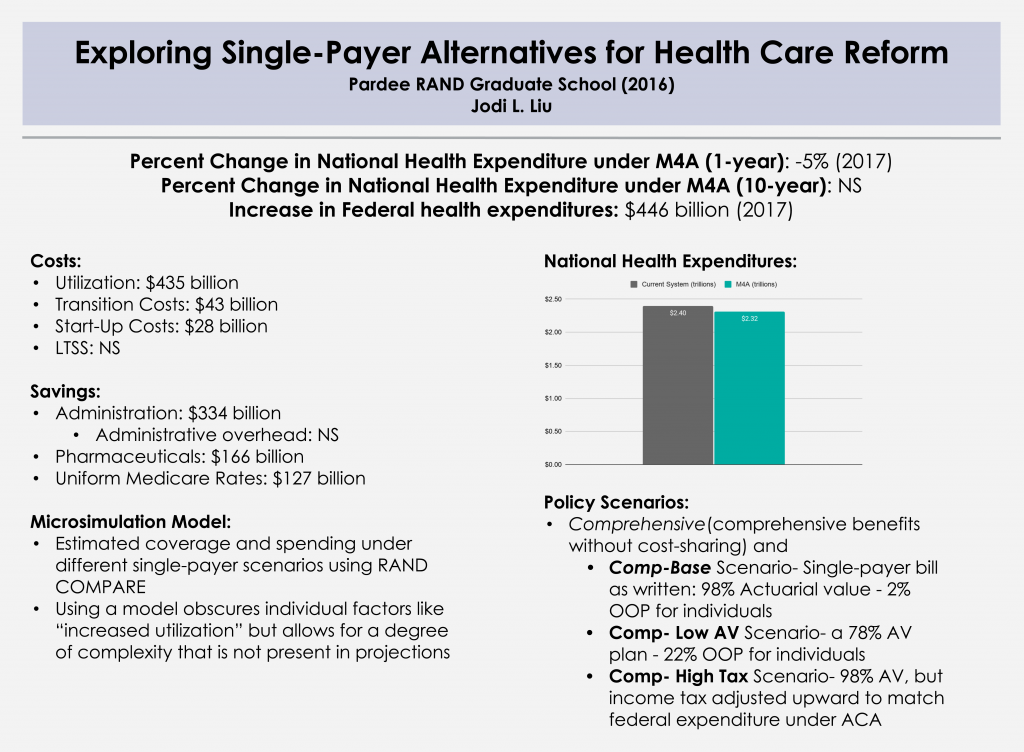
back to top“Exploring Single-Payer Alternatives for Health Care Reform”
RAND 2016
Title: Exploring Single-Payer Alternatives for Health Care Reform
Year: 2016
Authors: Jodi L. Liu
Institution: Pardee RAND graduate school
Funding Source: N/A
Plan Analyzed: S. 1782 / H.R. 1200
Percent Change in National Health Expenditure under M4A (1-year): -5% (2017)
Percent Change in National Health Expenditure under M4A (10-year): NS
Increase in Federal health expenditures: $446 billion (2017)
Read Study:
Exploring Single-Payer Alternatives for Health Care Reform
Study Abstract:
The Affordable Care Act (ACA) has reduced the number of uninsured and established new cost containment initiatives. However, interest in more comprehensive health care reform such as a single-payer system has persisted. Definitions of single-payer systems are heterogeneous, and estimates of the effects on spending vary. The objectives of this dissertation were to understand single-payer proposals and to estimate health care spending under single-payer alternatives in the United States. Single-payer proposals are wide-ranging reform efforts spanning financing and delivery, but vary in the provisions. I modeled two sets of national scenarios – one labeled comprehensive and the other catastrophic – and compared insurance coverage and spending relative to the ACA in 2017. First, I estimated the effects of utilization and financing changes, and then I added the effects of “other savings and costs” relating to administration, drug and provider prices, and implementation. Due to coverage of all legal residents and low cost sharing, and prior to adjusting for other savings and costs, the comprehensive scenario increased national health care expenditures by $435 billion and federal expenditures by $1 trillion relative to the ACA. The range of the net effect of the other savings and costs in the literature was $1.5 trillion in savings to $140 billion in costs, with a mean estimate of $556 billion in savings. If this mean estimate was applied to the comprehensive scenario, national expenditures would be $121 billion lower but federal expenditures would still be $446 billion higher relative to the ACA. The catastrophic scenario also covered all legal residents but increased overall cost sharing, resulting in a reduction in national expenditures by $211 billion and federal expenditures by $40 billion even before adjusting for other savings and costs. Average household spending on health care in both sets of scenarios could be more progressive by income than spending under the ACA. I also developed an interactive, web-based cost tool that allows the savings and cost assumptions to be adjusted by any user. As the debate on how to finance health care for all Americans continues, this study provides increased transparency about economic evaluations of health care reform.
Overview:
- This comprehensive 2016 paper served as Jodi Liu’s dissertation, which utilizes a microsimulation model to account for costs/savings and individual level variation
- The paper contains four main chapters:
- Chapter 1: A review of types of health care systems, single-payer systems worldwide, and brief overview of single-payer health care reform in the United States
- Chapter 2: Definitions of single-payer health care systems and a survey of single-payer proposals
- Chapter 3: Estimates of health insurance coverage and spending under single-payer scenarios
- Liu looks at 2 policy scenarios: Comprehensive (comprehensive benefits without cost-sharing) and Catastrophic (coverage only against large financial loss)
- Comp-Base Scenario – Single-payer bill as written: 98% Actuarial value (2% OOP for individuals)
- Comp-Low AV Scenario – a 78% AV plan (22% OOP for individuals)
- Comp-High Tax Scenario – 98% AV, but income tax adjusted upward to match federal expenditure under ACA
- Chapter 4: Description of a cost tool that could be used to understand assumptions (not available)
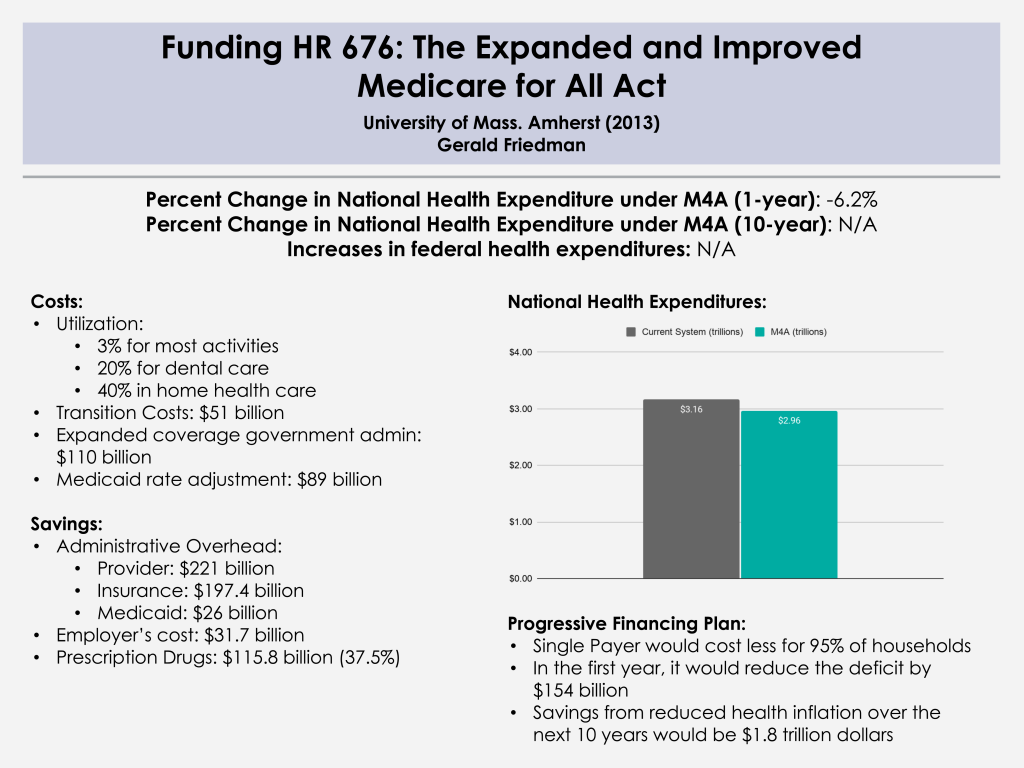
“Funding HR 676: The Expanded and Improved Medicare for All Act”
University of Massachusetts at Amherst 2013
Title: Funding HR 676: The Expanded and Improved Medicare for All Act
Year: 2013
Author: Gerald Friedman
Institution: University of Massachusetts at Amherst
Plan Analyzed: H.R. 676
Percent Change in National Health Expenditure under M4A (1-year): -6.2% (2014)
Read Study:
Funding HR 676: The Expanded and Improved Medicare for All Act
Abstract:
The Expanded and Improved Medicare for All Act, HR 676, introduced into the 113th Congress by Rep. John Conyers Jr. and 37 initial co-sponsors, would establish a single authority responsible for paying for medically necessary health care for all residents of the United States. Under the single-payer system created by HR 676, the U.S. could save an estimated $592 billion annually by slashing the administrative waste associated with the private insurance industry ($476 billion) and reducing pharmaceutical prices to European levels ($116 billion). In 2014, the savings would be enough to cover all 44 million uninsured and upgrade benefits for everyone else. No other plan can achieve this magnitude of savings on health care. Specifically, the savings from a single-payer plan would be more than enough to fund $343 billion in improvements to the health system such as expanded coverage, improved benefits, enhanced reimbursement of providers serving indigent patients, and the elimination of co-payments and deductibles in 2014. The savings would also fund $51 billion in transition costs such as retraining displaced workers and phasing out investor owned, for-profit delivery systems. Health care financing in the U.S. is regressive, weighing heaviest on the poor, the working class, and the sick. With the progressive financing plan outlined for HR 676 (below), 95% of all U.S. households would save money. HR 676 would also establish a system for future cost control using proven-effective methods such as negotiated fees, global budgets, and capital planning. Over time, reduced health cost inflation over the next decade (“bending the cost curve”) would save $1.8 trillion, making comprehensive health benefits sustainable for future generations.
Overview:
Dr. Friedman conducts an easy-to-follow cost analysis of H.R. 676 using a projection model. Dr. Friedman also discusses financing this program through both existing funding sources and “progressive taxation.”
- Section I: Financing needs for single payer
- Current regressive and obsolete funding sources to be replaced by progressive taxation
- Estimated costs of system improvements and transition costs
- Section II: Single-payer system savings as a source of financing
- Savings on provider administrative overhead and drug prices
- Savings on the administrative overhead of private insurers, Medicaid, and employers
- Section III: A progressive financing plan for HR 676 for 2014
- Conclusion: Single payer covers more, costs less for 95 percent of Americans
Further Reading:
Gordon Mosser Critical Review and comment by Dr. Don McCanne
back to topPre-ACA National Studies
- “Impacts of Health Care Reform: Projections of Costs and Savings” and supplemental slide set (National Coalition on Health Care, 2005)
- “Universal Coverage:How Do We Pay For It?” (Economic Policy Institute, 1998)
- “Preliminary Estimate of the Effects of S. 491, American Health Security Act of 1993, on Government Outlays and National Health Expenditures” (Congressional Budget Office, 1993)
- “Estimates of Health Care Proposals from the 102nd Congress” (Congressional Budget Office, 1993)
- “Single-Payer and All-Payer Health Insurance Systems Using Medicare’s Payment Rates” (Congressional Budget Office, 1993)
- “Universal Health Insurance Coverage Using Medicare’s Payment Rates” (Congressional Budget Office, 1991)
- “Canadian Health Insurance: Lessons for the United States” (General Accounting Office, 1991)
State Studies
- “Assessing the Costs and Impacts of a State-Level Universal Health Care System in Maine” (Maine Center for Economic Policy, 2019)
- “An Assessment of the New York Health Act: A Single-Payer Option for New York State” (RAND, 2018) and the subsequent critique/analysis, “What Can We Learn from RAND about What Single Payer Will Cost? And What Will It Save?” (Leonard Rodberg, 2018)
- “Economic Analysis of the Healthy California Single-Payer Health Care Proposal (SB-562)” (Political Economy Research Institute, 2017)
- “The Price of Single Payer: A Fiscal and Economic Analysis of the New York Health Act” (The Foundation for Research on Equal Opportunity, 2017)
- “A Comprehensive Assessment of Four Options for Financing Health Care Delivery in Oregon” (RAND, 2017)
- “Economic Analysis of the New York Health Act” (Gerald Friedman, University of Massachusetts at Amherst, 2015)
- “Cost and Economic Impact Analysis of a Single-Payer Plan in Minnesota” (Lewin Group, 2012)
- “Achieving Quality, Affordable Health Insurance for All New Yorkers: An Analysis of Reform Options” and press release (Urban Institute, 2009)
- “Lewin’s Technical Assessment of Health Care Reform Proposals” for the State of Colorado (Lewin Group, 2007)
- “Kansas – Pricing the Roadmap To Health Insurance Reform Options” (Schramm Raleigh Health Strategy, 2007)
- “The Health Care For All Californians Act: Cost and Economic Impacts Analysis” (Lewin Group, 2005)
- “The Georgia SecureCare Program: Estimated Cost and Coverage Impacts” (Lewin Group, 2003)
- “A Universal Health Care Plan for Missouri” (Missouri Foundation for Health, 2003)
- “Cost and Coverage Analysis of Nine Proposals to expand Health Insurance Coverage in California” (Lewin Group, 2002)
- “Feasibility of a Single-Payer Health Plan Model for the State of Maine” (Mathematica Policy Research, 2002)
- “The Feasibility of Consolidated Health Care Financing and Streamlined Health Care Delivery in Massachusetts” (LEGC, 2002)
- “Rhode Island Can Afford Health Care for All: A Report to the Rhode Island General Assembly” (Solutions for Progress and Boston University School of Public Health, 2002)
- “Analysis of the Costs and Impact of a Universal Health Care Coverage Under a Single Payer Model for the State of Vermont” (Lewin Group, 2001)
- “Analysis of the Costs and Impact of Universal Health Care Models for the State of Maryland: The Single-Payer and Multi-Payer Models” (Lewin Group, 2000)
- Two fiscal studies of single payer for the Massachusetts Medical Society available in their House of Delegates Report 207, A-99 (B). (Lewin Group and Solutions for Progress / Boston University School of Public Health, 1998)
- “Single-payer financing for Universal Health Care in Delaware: Costs and Savings” found that a single-payer system in the state would generate cumulative savings of more than $6 billion over 10 years (Solutions for Progress, prepared for the Delaware Developmental Disabilities Planning Council, 1995)
- “Health Care Administrative Costs” conducted for the Program Evaluation Division, Office of the Legislative Auditor, State of Minnesota (Lewin Group, 1995)
- “The Financial Impact of Alternative Health Reform plans in New Mexico” (Lewin Group, 1994)