As the COVID-19 pandemic wreaks physical and financial havoc across the United States, PNHP members have been writing op-eds and letters to the editor demanding long overdue single-payer reform. Members have also been appearing on television programs, radio shows, online video segments, and podcasts.
Interested in developing your own letter or op-ed? See our detailed suggestions on writing and submitting, or contact PNHP communications specialist Clare Fauke at clare@pnhp.org.
Television and radio segments
Coronavirus and Health Inequities
Interview with former APHA president Dr. Linda Rae Murray
JAMA Live, June 19, 2020
“We’re going to be dealing with Coronavirus for a while”
Interview with PNHP-MO chair Dr. Ed Weisbart
KTRS Radio, June 10, 2020
Millions of out-of-work Americans lose their health insurance
Featuring PNHP president Dr. Adam Gaffney and Dr. Victoria Dooley
CBC News, The National, May 15, 2020
How America’s Health Workers Lack Adequate Health Care
Interview with PNHP co-founder Dr. Steffie Woolhandler
Rising Up With Sonali, April 29, 2020
Coronavirus: One thing that makes job loss in U.S. so painful
Featuring PNHP co-founder Dr. Steffie Woolhandler
BBC News, April 28, 2020
13 Million will be added to the list of uninsured by June
Interview with PNHP co-founder Dr. Steffie Woolhandler
WORT Community Radio (Madison, Wisc.), April 15, 2020
Coronavirus Triggered Unemployment Leads to Massive Loss of Health Insurance Coverage
Interview with PNHP co-founder Dr. Steffie Woolhandler
Between the Lines, April 15, 2020
The Folly of Employer-based Health Insurance with 47 Million Unemployed
Interview with PNHP co-founder Dr. Steffie Woolhandler
Background Briefing with Ian Masters, April 9, 2020
The impact of Coronavirus on public health, and the need for Medicare for All
Interview with PNHP-MO chair Dr. Ed Weisbart
KTRS Radio, April 7, 2020
Meet This Moment With Medicare For All
Interview with PNHP national board member Dr. Paul Song and Business for Medicare for All president Wendell Potter
The Robust Opposition, April 6, 2020
Coronavirus could hit low-income, minority communities harder due to health care disparities
Interview with PNHP national coordinator Dr. Claudia Fegan and PNHP president-elect Dr. Susan Rogers
WGN News, April 1, 2020
‘Everyone is afraid’ as Illinois virus cases spike
Interview with PNHP national coordinator Dr. Claudia Fegan
PBS NewsHour, March 30, 2020
Behind the News Podcast: COVID-19
Featuring PNHP co-founder Dr. David Himmelstein (at 7:20)
Jacobin Radio, March 25, 2020
The Issue Is: Coronavirus
Interview with PNHP national board member Dr. Paul Song
The Issue Is, March 21, 2020
Biden Is Wrong—Single-Payer Healthcare Does Help Fight Pandemics
Interview with Dr. James Kahn
The Real News Network, March 19, 2020
Roundtable: Coronavirus Shows the Need for Medicare for All
Featuring PNHP co-founder Dr. Steffie Woolhandler
Democracy Now, March 5, 2020
Coronavirus Spread and the Urgent Need for Medicare for All
Interview with PNHP national board member Dr. Paul Song
Rising Up With Sonali, February 26
News and opinion pieces
U.S. health insurers doubled profits in second quarter amid pandemic
Quotes PNHP co-founder Dr. Steffie Woolhandler
The Guardian, August 14, 2020
The enormous medical response in America to the coronavirus pandemic has not put a drain on US health insurers, which doubled profits in the second quarter of 2020 compared with the same time last year. Continue reading…
US doctor in Canada: Medicare for All would have made America’s COVID response much better
By Dr. Khati Hendry
USA Today, August 5, 2020
I’m a family physician who moved to Canada from California 14 years ago, largely because of Canadian Medicare, the country’s national health insurance program. I’ve been much happier practicing medicine where my patients have universal coverage. Continue reading…
More people called out sick in April than at any time on record. Was it COVID-19?
Quotes PNHP president Dr. Adam Gaffney
McClatchy News Service, July 28, 2020
When the novel coronavirus planted its feet firmly in American soil around March, the amount of people calling out sick from work grew to the highest number since at least 1976, according to new research, suggesting the number of COVID-19 cases is far greater than reported. Continue reading…
Record-Breaking Number of Americans Called Out Sick From Work in April, Study Finds
Quotes PNHP president Dr. Adam Gaffney
Gizmodo, July 27, 2020
New research out Monday may provide more insight into how many Americans were sickened by covid-19 during the earliest days of the pandemic, when access to testing was extremely limited. Continue reading…
Pandemic reveals big need for universal health care
By Erica Heiman, M.D.; Jack Bernard; and Henry Kahn, M.D.
The (Jacksonville) Florida Times-Union, July 14, 2020
COVID-19 has stolen the lives of over 130,000 Americans so far with many more to come. We think that universal health insurance coverage — such as expanded, improved Medicare for All — would have lessened the pandemic’s impact on our nation. Continue reading…
Our Health Care Is ‘Market Chaos’
Interview with PNHP president Dr. Adam Gaffney
Democracy, Voices of the Virus, June 26, 2020
There’s no question that the epidemic intensified the debate about health-care reform in this country. It clearly laid bare many of the dysfunctions and the injustices of the U.S. way of paying for health care. Continue reading…
Pandemic response shows glaring health care finance inequities
By PNHP board adviser Dr. Robert Stone
The (Fort Wayne, Ind.) Journal Gazette, June 25, 2020
Follow the money. The coronavirus spread like wildfire across the United States. New York City hospitals were quickly overwhelmed with sick and dying patients. Everywhere, hospitals scrambled to create more ICU beds and find more ventilators. Continue reading…
Millions at high risk of severe COVID-19 outcomes lack coverage to cover costs
Quotes PNHP president Dr. Adam Gaffney
Modern Healthcare, June 10, 2020
More than 18 million people who were most at risk of experiencing severe outcomes from COVID-19 at the start of the outbreak had the least access to healthcare because they were either uninsured or underinsured. Continue reading…
18 Million Americans Lack Adequate Health Insurance While Facing Greater Risk of Severe Coronavirus, Study Finds
Quotes PNHP president Dr. Adam Gaffney and PNHP co-founder Dr. Steffie Woolhandler
Newsweek, June 10, 2020
More than 18 million Americans, most of whom are minorities and low-income individuals, are uninsured or underinsured while also being at increased risk of developing severe cases of COVID-19. Continue reading…
The other epidemic: Lack of health insurance for all Americans
By Health Care Justice—NC chair Dr. Jessica Schorr Saxe
The Charlotte Post, May 27, 2020
Rapidly and predictably following the onset of the pandemic, many Americans are victims of an epidemic of uninsurance, which will also predictably lead to suffering and death. Continue reading…
The Coronavirus Isn’t the Only American Health Epidemic
By Dr. Augie Lindmark
The Nation, May 21, 2020
Lately my work in the hospital consists of two activities. Admit patients with Covid-19, and, if lucky, discharge patients with Covid-19. Continue reading…
COVID-19 and Medicare for All
By Drs. Ashley Duhon and Sara Robicheaux
The Lens, May 21, 2020
Last week, we officially began our careers as physicians in the middle of a global pandemic and public health crisis. Continue reading…
Best of times, worst of times
By Dr. Robert S. Kiefner
Concord (N.H.) Monitor, May 16, 2020
With the opening paragraph of “The Tale of Two Cities,” Charles Dickens provided an overview of our new reality; our lives in the time of COVID-19. Continue reading…
Inmates and Staff Fearful as Coronavirus Strikes Prisons, Jails
Quotes PNHP co-founder Dr. Steffie Woolhandler
MedPage Today, April 30, 2020
Coronavirus outbreaks in prisons and jails across the country have the potential to cripple any gains made by local communities in curbing the pandemic. “They’re not some isolated spot where you can just stick people.” Continue reading…
In U.S., more than 1 in 4 healthcare workers lack paid sick leave – study
Quotes PNHP co-founders Drs. David Himmelstein and Steffie Woolhandler
Reuters, April 29, 2020
Many U.S. healthcare workers on the front lines in the COVID-19 pandemic lack basic health insurance and more than 1 in 4 have no paid sick leave, increasing the risk that they will show up for work even if they are infected with the coronavirus. Continue reading…
Coronavirus throws spotlight on American health care
By Dr. Mary Ganguli and Judith R. Lave
Pittsburgh Post-Gazette, April 29, 2020
The coronavirus pandemic has spread across the world. Watching the news shows us how this health care crisis is playing out in different countries with their different political systems and health care financing systems. Continue reading…
COVID-19 crisis bring light to insurance disparities
By Columbia (Mo.) health care providers
The Missourian, April 21, 2020
Millions of Americans rely on employment-based health insurance, but problems caused by the linkage of insurance to employment are increasingly evident. Continue reading…
Early pandemic health lessons
By Dr. James G. Fieseher
SeacoastOnline.com, April 17, 2020
Much will be written about the lessons learned from the COVID-19 pandemic. Here are a few I have observed at this time in the process. Continue reading…
Profit over people, cost over care: America’s broken healthcare exposed by virus
Quotes PNHP president Dr. Adam Gaffney
The Guardian, April 16, 2020
With over 30,900 people dead and more than a 639,000 infected with the coronavirus in the US the last question on a person’s mind should be how they will pay for life-saving treatment. Continue reading…
U.S. for-profit health care sector cuts thousands of jobs as pandemic rages
Quotes PNHP co-founder Dr. David Himmelstein
The Guardian, April 14, 2020
Maureen Zeman was a registered nurse for 29 years at a hospital in San Jose, California, before she was laid off with dozens of other nurses despite the coronavirus pandemic. Continue reading…
As economy sheds jobs, bring on Medicare for all the unemployed
By Dr. George Bohmfalk
The Charlotte Observer, April 13, 2020
As a result of the coronavirus pandemic, millions of U.S. workers who were satisfied with and didn’t want to give up their employer-provided health insurance are losing both their jobs and the associated insurance. Continue reading…
Employer-based insurance is a crumbling defense against a global pandemic
By Jordan Rook, Alec Feuerbach, and Jake Fox
The Colorado Sun, April 13, 2020
The losses inflicted by SARS-Cov-2, the novel coronavirus that causes COVID-19, have been staggering. In the U.S., over 555,000 have fallen ill, more than 22,000 have perished, and even our most optimistic models suggest… Continue reading…
The health-care pandemic
By PNHP past president Dr. Johnathon Ross
The Toledo (Ohio) Blade, April 10, 2020
For centuries, public health experts have known that contagious, deadly diseases like measles, polio, hepatitis, HIV, tuberculosis, flu — and now coronavirus — are much more difficult and expensive to treat than to prevent. Continue reading…
“This Is A World-Changing Event”
Interview with PNHP past president Dr. Andy Coates
WAMC, The Roundtable, April 10, 2020
I guess I’m losing track of the weeks, two or three, four weeks. There has been an eerie calm with the command for social distancing. Continue reading…
In Chicago, 70% of COVID-19 Deaths Are Black
Quotes former APHA president Dr. Linda Rae Murray
WBEZ, April 5, 2020
The COVID-19 virus is killing black residents in Cook County at disproportionately high rates, according to early data analyzed by WBEZ. While black residents make up only 23% of the population in the county, they account for 58% of the COVID-19 deaths. Continue reading…
How a pandemic makes the most compelling case for ‘Medicare for All’
Quotes Drs. Marcia Angell and Donald Moore
Well + Good, April 3, 2020
Medicare for All has been shoved front and center as public support for universal health care surges amid the COVID-19 pandemic. In the last two weeks, millions of Americans have lost their jobs—and with them, their health insurance. Continue reading…
Hospitals Got $100 Billion in the Stimulus Package. But A Lot of That Could Go Toward Administrative Costs
Quotes PNHP co-founder Dr. Steffie Woolhandler
TIME, April 1, 2020
Hospitals have spent the past few weeks racing to respond to the growing COVID-19 crisis, supplementing shortages of equipment, calling back retired personnel, and transforming entire hospital wings to care for infected patients. Continue reading…
Universal health care would benefit state amid COVID-19
By Dr. Samuel Metz
Portland (Ore.) Tribune, April 1, 2020
Oregon’s Universal Health Care task force, charged by our Legislature to design a statewide health care insurance plan, canceled its first meeting when COVID-19 spread across the state. Continue reading…
ICU doctor: Coronavirus frightens me. It’s severe, unpredictable and it has no cure.
By PNHP national board member Dr. Phil Verhoef
USA Today, March 26, 2020
The shift from trying to contain the illness to treating those who have been infected, one at a time, is eye opening and heart rending. What do you do when there are vastly more sick patients than you can care for? Continue reading…
US private health insurance companies clog system amid Covid-19 pandemic
Quotes former SNaHP board member Dr. Augie Lindmark
The Guardian, March 26, 2020
As Augie Lindmark, a resident physician at Yale University prepared for an onslaught of Covid-19 patients last week, he noticed something at his hospital: there were still patients without the virus, completely stable, in the beds. Continue reading…
Why are we waiting for Medicare for All?
By F. Douglas Stephenson, LCSW, BCD
The Gainesville (Fla.) Sun, March 23, 2020
An old social justice chant, “Why are We Waiting,” is sung to the tune of the beautiful and inspiring Christmas carol, “O Come All Ye Faithful.” The lyrics apply to the situation today. Continue reading…
America’s extreme neoliberal healthcare system is putting the country at risk
By PNHP president Dr. Adam Gaffney
The Guardian, March 21, 2020
At the final debate of the Democratic presidential primary on Sunday, Senator Bernie Sanders and Joe Biden clashed on the coronavirus. Sanders contended the pandemic laid bare “the incredible weakness and dysfunctionality” of the US healthcare system, and called for single-payer reform. Continue reading…
Why the U.S. failed the coronavirus test
By former New England Journal of Medicine editor-in-chief Dr. Marcia Angell
Santa Fe New Mexican, March 21, 2020
The coronavirus pandemic is the best argument for “Medicare for All.” As it stands, most Americans get health care only if we have insurance that will pay for it. If we don’t or we can’t afford the deductibles and copayments, too bad. Continue reading…
COVID-19 pandemic proves need for Medicare for all
By PNHP Cincinnati co-founder Dr. James Binder
The Cincinnati Inquirer, March 20, 2020
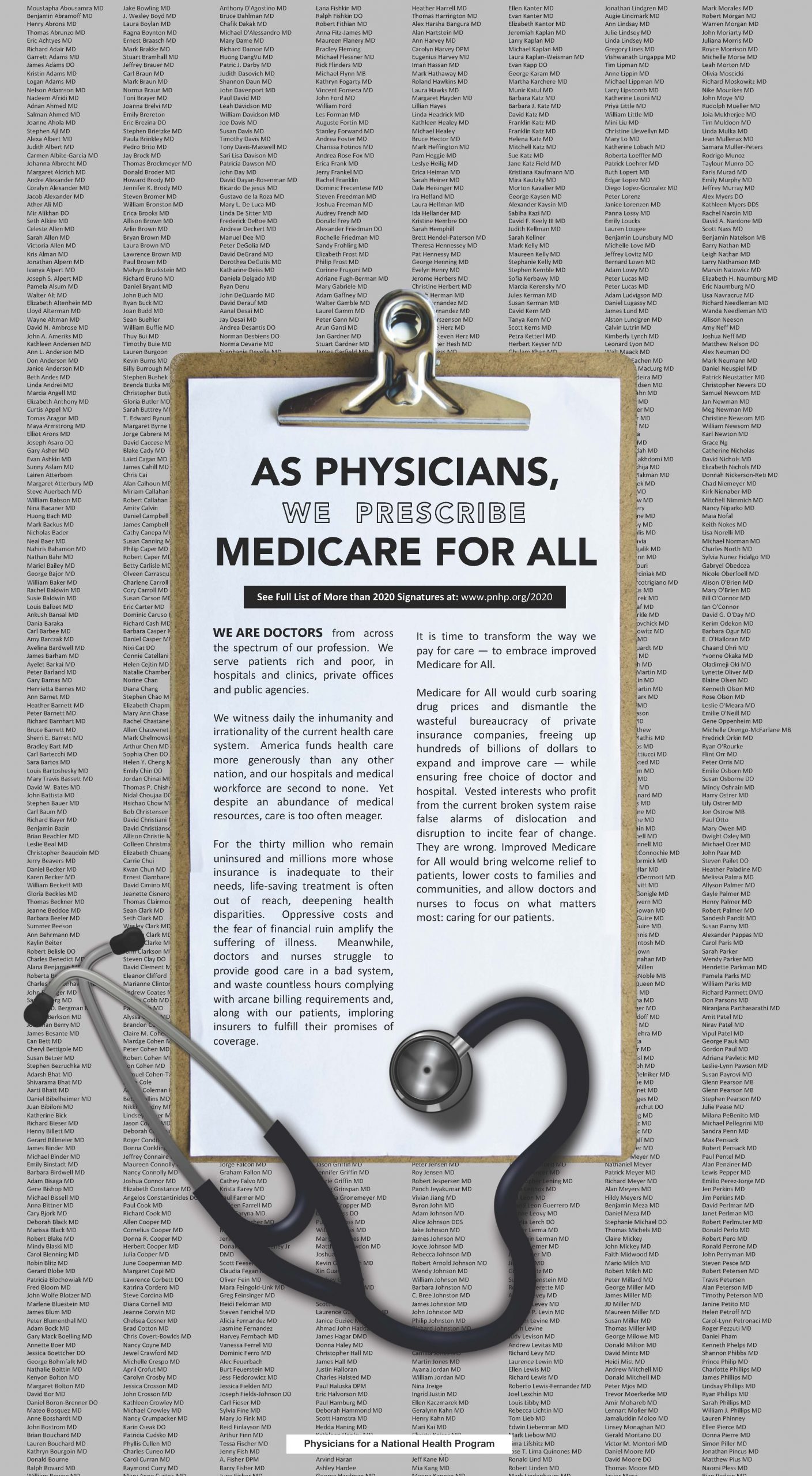
I am one of the 23,000 members of the Physicians for a National Health Program (PNHP) who advocate for Medicare for all. Our current health crisis provides strong evidence that we indeed do need a Medicare for all system in this country. Continue reading…
Masks, Gowns, and Medicare For All
By Jonathan Michels
Piedmont Left Review, March 20, 2020
If patients want to support healthcare workers on the frontlines of the coronavirus pandemic, they should join us in calling for a universal, single-payer healthcare system. Continue reading…
Coronavirus: A strong argument for Medicare for All
By Dr. Alice Rothchild
The Seattle Times, March 18, 2020
COVID-19 has laid bare the weaknesses in our system and the urgent need for Medicare for All. We cannot nationally isolate or personally buy our way out of this outbreak. Continue reading…
Public Health Experts: Single-Payer Systems Coping With Coronavirus More Effectively Than For-Profit Model
Quotes PNHP co-founder Dr. David Himmelstein
Common Dreams, March 16, 2020
As the coronavirus pandemic places extraordinary strain on national health care systems around the world, public health experts are making the case that countries with universal single-payer systems have thus far responded more efficiently and effectively to the outbreak than nations like the United States. Continue reading…
Love in the time of coronavirus
By Dr. Dipesh Navsaria
Madison (Wisc.) State Journal, March 16, 2020
Universal health care is a form of love for others as well — not only does it speak to a societal belief that we all deserve to be healthy, but it ensures that a lack of health coverage doesn’t result in greater spread of disease due to delayed diagnosis. Continue reading…
Surprise medical bills, coronavirus and bad insurance: 3 arguments for Medicare for All
By PNHP national board member Dr. Phil Verhoef
USA Today, March 9, 2020
Working in various hospitals across the country, I have met so many patients who delay or avoid needed care for fear of surprise bills and financial catastrophe. That’s risky for them and, in the face of a threat like coronavirus, for all of us. Continue reading…
Letters to the editor
Covid-19 pandemic demands better health care coverage
By Dr. Robert Milch
The Buffalo News, August 4, 2020
While the pandemic rages, our President touts a questionable mortality rate under 2% as some perverse indicator, 136,000 deaths later, that “things are under control.” Continue reading…
Medicare for All amid a pandemic
By George Bohmfalk, M.D.
The Charlotte Observer, Letters, July 27, 2020
Until now, rationing has only been a scare tactic in criticisms of Medicare for All. Our free-market, capitalistic, for-profit health care system promised to spare us from socialist disasters like rationing. Continue reading…
What the C.D.C. Did Wrong, and Why
By Drs. Malini DeSilva, Philip Lederer, and Brian Yablon
New York Times, June 4, 2020
The C.D.C. is a leading international public health entity, its programs and projects drive health policy, and it responds to outbreaks of public health significance worldwide. Despite all of this, the agency, along with state and local health departments, has been underfunded and neglected for decades. Continue reading…
COVID-19 exposes flaws of employer-based health insurance
By Jack Bernard, former Director of Health Planning for the state of Georgia
Modern Healthcare, May 16, 2020
Before the COVID-19 pandemic, the U.S. was the worst-performing developed nation regarding health insurance coverage, with 45% underinsured or uninsured despite the Affordable Care Act. Continue reading…
The coronavirus highlights Obamacare’s glaring shortcomings
By Dr. Jay D. Brock
Washington Post, May 12, 2020
Defending the ACA is ultimately an exercise in futility because the ACA will not fix the two glaring problems besetting health insurance today: lack of universal coverage and affordability. Continue reading…
Time for single-payer health care
By Sachin Jindal
The (Toledo, Ohio) Blade, May 9, 2020
To prepare for a future pandemic, it is clear that the United States must transition to a federally funded single-payer health-care system. Continue reading…
Crisis highlights need for universal health care
By Dr. Robert Blake
St. Louis Post-Dispatch, May 3, 2020
Millions of Americans depend on employment-based health insurance, but problems caused by the linkage of insurance to employment are increasingly evident. Continue reading…
COVID-19’s impact on health insurance
By Dr. Kathleen Healey
Napa Valley (Calif.) Register, April 28 2020
Millions in our nation have just lost their jobs and their family’s health insurance in the middle of a COVID-19 pandemic. These families not only face the prospect of illness, but enormous medical expenses. Continue reading…
Hospital cutbacks amid coronavirus accentuate the flaws in our health care system
By former SNaHP board member Jonathan Michels
Raleigh News & Observer, April 10, 2020
The coronavirus pandemic lays bare the ways in which our expensive, inefficient and profit-driven health care system has left our communities defenseless against public health crises. Continue reading…
Protect workers, provide health coverage
By Joyce Schlag, CCW
Pittsburgh Post-Gazette, Letters, March 19, 2020
We are all connected, a community of people experiencing vulnerability in the face of the coronavirus which threatens us, our families, neighbors and friends. We are becoming aware of how the well being of one person can affect the well being of many. Continue reading…
Everyone must take this virus seriously
By Dr. George Bohmfalk
The Charlotte Observer, Letters, March 16, 2020
Fellow citizens, please take this seriously. Even young, healthy people can die from this. You can carry it to your elderly parents and grandparents. Stay home unless absolutely necessary. Keep your distance in public. Wash those hands, often. Use common sense for everyone’s sake. Continue reading…
Improved Medicare for All will keep us safer
By Bill Semple, board chair, Colorado Foundation for Universal Health Care
Daily Camera (Boulder, Colo.), Letters, March 13, 2020
Our current patchwork of health care coverage, with its gaps, bureaucratic obstacles, high deductibles, co-pays, surprise billings, prior authorizations, claims denials, stagnant wages and narrow networks of providers leave us vulnerable. Continue reading…
Americans need a fully funded health care program
By PNHP Western Pennsylvania co-founder Dr. Judy Albert
Pittsburgh Post-Gazette, Letters, March 9, 2020
The coronavirus has arrived in the U.S. and it’s only a matter of time before it reaches Western Pennsylvania. The American public copes with fear of infection by stockpiling hand sanitizer, rather than considering how this epidemic demonstrates the unavoidable connection we have with one another and with all living things on the planet. Continue reading…
Support Medicare for All
By Dr. Kathleen Healey
San Francisco Chronicle, Letters, March 9, 2020
Americans are threatened by a COVID-19 pandemic and over 27 million of us have no health insurance. What could possibly go wrong? During an outbreak of a communicable disease we are all safer if everyone around us has access to health care. Continue reading…
Quote of the day
For more recent entries (after June 30, 2020) please see the QOTD page on our website. You may also wish to subscribe to the QOTD mailing list to receive daily emails.
Americans want the option of a government-regulated and -subsidized health plan
Comment by Dr. Don McCanne
Quote of the Day, June 23, 2020
Although most of the questions in this latest poll were about job loss and insurance coverage, plus some questions about public policies during the COVID pandemic, the question above stood out. Continue reading…
Hannity’s downplaying of COVID-19 threat increased deaths
Comment by Dr. Don McCanne
Quote of the Day, June 22, 2020
Do television hosts have a responsibility when they disseminate misinformation that results in adverse consequences on the viewing audience? Continue reading…
V. Fuchs: We may now have the dynamic for political change in health reform
Comment by Dr. Don McCanne
Quote of the Day, June 15, 2020
For decades, Victor Fuchs has been telling us, “National health insurance will probably come to the United States after a major change in the political climate — the kind of change that often accompanies a war, a depression, or large-scale civil unrest.” Continue reading…
COVID-19 crisis comes with financial toxicity
Comment by Dr. Don McCanne
Quote of the Day, June 12, 2020
As Steffie Woolhandler states, “Medicare for All is the long-term answer.” Continue reading…
COVID-19 and Health Financing: Perils and Possibilities
Comment by Dr. Don McCanne
Quote of the Day, June 10, 2020
Although we have the most expensive health care system in the world, the COVID-19 pandemic provides stark evidence that our health care financing system is highly dysfunctional, wasting tremendous resources while impairing health care access. Continue reading…
Hospital CEOs paid millions while many workers furloughed
Comment by Dr. Don McCanne
Quote of the Day, June 8, 2020
Billions of dollars of taxpayer funds have been paid out to some of the nation’s largest and most successful hospital chains, supposedly to prevent job losses of health care workers, though tens of thousands have instead received pay cuts or have even been furloughed. Continue reading…
Challenging inequality through the ‘civil rights of health’
Comment by Dr. Don McCanne
Quote of the Day, June 4, 2020
We have read much about the social determinants of health and the social and economic inequities that lead to unjust health disparities. As these authors state, “justice makes us healthy and injustice makes us ill.” Continue reading…
China’s delay, WHO’s frustration, and US’s abdication
Comment by Dr. Don McCanne
Quote of the Day, June 2, 2020
President Trump has recently condemned both China and the World Health Organization for their alleged delays and mismanagement of the COVID-19 pandemic. Continue reading…
AMA statement on Trump severing ties with WHO
Comment by Dr. Don McCanne
Quote of the Day, June 1, 2020
President Trump’s effort to sever ties with the World Health Organization during this horrendous pandemic seems like it screams out for nonviolent resistance. Continue reading…
Bailout funds go to the wealthiest hospitals
Comment by Dr. Don McCanne
Quote of the Day, May 26, 2020
Compared to our highly dysfunctional, fragmented system of financing health care, heavily dependent on private health insurance, a single payer model of an improved Medicare program that covered everyone would be vastly superior. Continue reading…
COVID-19 vaccine as a ‘global public good’
Comment by Dr. Don McCanne
Quote of the Day, May 21, 2020
At the virtual meeting of the World Health Organization this week, China expressed its intent to produce a much needed COVID-19 vaccine as a “global public good.” Continue reading…
Balanced budget requirements threaten Medicaid program
Comment by Dr. Don McCanne
Quote of the Day, May 19, 2020
The COVID-19 pandemic combined with a major economic downturn, massive loss of employment, often with the loss of health insurance, has resulted in much greater demand for enrollment in the Medicaid program. Continue reading…
What should we do about the payer-provider disconnect?
Comment by Dr. Don McCanne
Quote of the Day, May 15, 2020
The current pandemic certainly demonstrates the payer-provider disconnect in health care. The private insurers are doing spectacularly well whereas the players in the health care delivery system – many hospitals and especially physicians – are facing a financial crisis. Continue reading…
Rich hospitals get government handouts
Comment by Dr. Don McCanne
Quote of the Day, May 14, 2020
Private insurers generally pay hospitals at twice the rate that Medicare pays and at an even greater multiple than what Medicaid pays. Continue reading…
Why would states deny retroactive eligibility for Medicaid?
Comment by Dr. Don McCanne
Quote of the Day, May 13, 2020
In the absence of a universal health care financing program it is inevitable that many will remain uninsured because they do not qualify for whatever programs are available, or they simply cannot afford them. Continue reading…
Is it time to nationalize hospitals?
Comment by Dr. Don McCanne
Quote of the Day, May 12, 2020
The combination of a health crisis plus an economic crisis that has disrupted the lives of everyone of us certainly lays fertile ground for reassessing our health care system and its financing. Continue reading…
Get sick now; Insurer fee waivers for COVID-19 treatment may expire by June 1
Comment by Dr. Don McCanne
Quote of the Day, May 8, 2020
The nation’s private health insurers now have a chance to prove to us that they are worthy of controlling our health expenditures. During the worst pandemic in a century, combined with a catastrophic economic downturn, what are they offering us? Continue reading…
WFTU on business games related to the COVID-19 vaccine
Comment by Dr. Don McCanne
Quote of the Day, May 7, 2020
Pretty strong statement. But, you know, we’ve been speaking for decades about the terrible deficiencies in our health care financing system. Continue reading…
Frank talk about the need for Medicare for All
Comment by Dr. Don McCanne
Quote of the Day, May 5, 2020
Sometimes it just needs to be said. Continue reading…
Covid-19 and Hospital Inequality
By Richard N. Gottfried, author of the New York Health Act
Quote of the Day, May 4, 2020
This article on hospital inequality in the COVID-19 epidemic is an excellent analysis by Barbara Caress, a long-standing keen analyst of our health care system. Continue reading…
Our safety net is a sieve with large rents
Comment by Dr. Don McCanne
Quote of the Day, May 1, 2020
The COVID-19 pandemic is bringing home the reality that it is imperative that our government always be at the ready to provide safety net functions in times of need, whether individual or societal. Continue reading…
‘Alliance to Fight for Health Care’ plans to defeat Medicare for All
Comment by Dr. Don McCanne
Quote of the Day, April 29, 2020
One of the painful lessons of the tragic Covid-19 pandemic is that we see how terrible the functioning of our health care financing system is, as if it weren’t already obvious before the pandemic arrived. Continue reading…
U.S. will not take part in WHO global drugs, vaccine initiative launch
Comment by Dr. Don McCanne
Quote of the Day, April 27, 2020
Talk about a time that we need to join together in international cooperation; we have a pandemic that has already caused over 200,000 deaths and economic disruption throughout the world. Continue reading…
Austerity and the Americanization of health care was Italy’s problem
Comment by Dr. Don McCanne
Quote of the Day, April 24, 2020
Italy’s lesson? Austerity kills. Continue reading…
Pandemic brings fallacy of insurance choice into focus
Comment by Dr. Don McCanne
Quote of the Day, April 21, 2020
The COVID-19 pandemic has certainly captured the attention of the media, and everyone else. How could it not, considering the dramatic adverse impact it has had on each of us? Continue reading…
What would Jonas Salk say?
Comment by Dr. Don McCanne
Quote of the Day, April 20, 2020
Understandably, much is being written about the lessons of the COVID-19 pandemic, particularly on how important it would be to have had in place an efficient and effective universal health program such as single payer Medicare for All. Continue reading…
Private agent vs. social planner in COVID-19 mitigation
Comment by Dr. Don McCanne
Quote of the Day, April 16, 2020
These two timely papers on the coronavirus pandemic should be of interest to single-payer supporters. Continue reading…
ACO wonks stumbling through the pandemic
Comment by Dr. Don McCanne
Quote of the Day, April 15, 2020
Earlier this week the National Association of ACOs released the results of a survey indicating that “a large portion of risk-based ACOs are likely to quit over concerns about COVID-19.” Continue reading…
Financial Times on the social contract
Comment by Dr. Don McCanne
Quote of the Day, April 14, 2020
It has become obvious to many of us that the government must play a greater role in establishing policies that allow us to advance a social contract that benefits everyone. Continue reading…
COVID-19: The swan song of ACOs
Comment by Dr. Don McCanne
Quote of the Day, April 13, 2020
Accountable Care Organizations (ACOs) were established on the theory that by making providers accountable for the health care they were providing, you could improve quality while lowering costs. Continue reading…
Malcolm Gladwell: The lesson of the COVID-19 pandemic
Comment by Dr. Don McCanne
Quote of the Day, April 10, 2020
“You know who should be leading the conversation about the health of our population? The public health people. They’re the ones. They have the most important lessons to teach us.” Continue reading…
COVID-19 pandemic and the loss of health insurance
Comment by Dr. Don McCanne
Quote of the Day, April 7, 2020
“National health insurance will probably come to the United States after a major change in the political climate — the kind of change that often accompanies a war, a depression, or large-scale civil unrest.” Continue reading…
Fate of commercial insurance under the COVID-19 pandemic
Comment by Dr. Don McCanne
Quote of the Day, April 6, 2020
Although we already have an inequitable, fragmented, dysfunctional health care financing system, in spite of the highest per capita health care spending of all nations, the current COVID-19 pandemic crisis is revealing the severe instability in our health care financing infrastructure. Continue reading…
Another gift of COVID-19: Medical bankruptcy
Comment by Dr. Don McCanne
Quote of the Day, April 1, 2020
As of 2020, our national health expenditures are $4 trillion, or $12,118 per capita. Considering that we are already spending that much, you would think that everyone could receive health care without experiencing financial hardship. Continue reading…
Saez and Zucman explain how we can protect our health and save our economy
Comment by Dr. Don McCanne
Quote of the Day, March 31, 2020
Much has been written about how having an equitable, efficient, comprehensive national health program (i.e., single payer Medicare for All) would have been extremely helpful combating illnesses caused by the coronavirus pandemic. Continue reading…
You don’t need a pandemic to lose your health plan at work
Comment by Dr. Don McCanne
Quote of the Day, March 27, 2020
A well designed single payer model of an improved Medicare for All would meet the health care financing needs of everyone forever while being affordable for each of us based on our ability to pay. Continue reading…
Emergency coronavirus funds for American Indians languish in bureaucratic limbo
Comment by Dr. Don McCanne
Quote of the Day, March 20, 2020
The Trump administration has held up $40 million in emergency aid Congress approved earlier this month to help American Indians combat the coronavirus. Continue reading…
GOP-led states diverge on easing Medicaid access during COVID-19
Comment by Dr. Don McCanne
Quote of the Day, March 19, 2020
You would think that the COVID-19 pandemic would provoke state administrators to look for ways of reducing barriers to health care. Expanding Medicaid coverage for low-income individuals would seem to be a logical step. Continue reading…
Can we put partisan politics aside during the pandemic?
Comment by Dr. Don McCanne
Quote of the Day, March 18, 2020
Unfortunately, President Trump did not get off to a sterling start in his response to the coronavirus crisis. He first wanted to minimize it so as to not distract from his campaign for reelection, and then when it appeared to be a more serious problem, he seemed more concerned about its impact on the economy rather than the potentially disastrous consequences that it would have on the health of the people. Continue reading…
Pandemics and Medicare for All
Comment by Dr. Don McCanne
Quote of the Day, March 17, 2020
Two issues were appropriately conflated during the Biden/Sanders debate. One is that nations must be prepared at all times to address current and future public health crises, and the other is that the United States needs to reform its health care financing infrastructure to make it work well for everyone. Continue reading…
Taiwan’s COVID-19 lesson for us
Comment by Dr. Don McCanne
Quote of the Day, March 13, 2020
Taiwan has a single payer national health program. The United States does not. Both nations now face the COVID-19 pandemic. “Taiwan is an example of how a society can respond quickly to a crisis and protect the interests of its citizens. (JAMA)” Yet in the United States, “The federal response really has been a fiasco. (Jha)” Continue reading…
With Coronavirus, ‘Health Care for Some’ Is a Recipe for Disaster
Comment by Dr. Don McCanne
Quote of the Day, March 12, 2020
Why should we have “a safety net big enough, and strong enough, for everyone” only during an epidemic? Every day people face potential financial hardship, suffer from injury and illness and perhaps die prematurely. Continue reading…