On May 17, 2023, Rep. Pramila Jayapal, Rep. Debbie Dingell, and Sen. Bernie Sanders introduced the Medicare for All Act in the U.S. House (H.R. 3421) and U.S. Senate (S. 1655). These landmark pieces of legislation would finally establish a single-payer national health program in the United States.
PNHP welcomes these bills and urges Congress to move quickly to guarantee universal coverage, comprehensive benefits, and zero out-of-pocket costs for all U.S. residents.
Overview of the Medicare for All Act
- Brief summaries covering major features of the House bill and Senate bill
- In-depth summary covering each section of the House Bill
- Medicare for All fact sheet providing context for the Senate bill
- PNHP’s news release celebrating the launch of the Medicare for All Act, as well as news releases from lead sponsors Rep. Pramila Jayapal and Sen. Bernie Sanders
- Full text of the Medicare for All Act (H.R. 3421, U.S. House)
- Full text of the Medicare for All Act (S. 1655, U.S. Senate)
Activism on the Medicare for All Act
- Send an email to your representative and and ask them to co-sponsor the bill.
- Call your representative and senators at (202) 224-3121 and ask them to co-sponsor.
- Schedule an in-person meeting with your representative and with each of you senators—or with a health policy staffer at their district office; this is a crucial part of building relationships with your legislators.
- If your representative or senator is already a co-sponsor, thank them for their support and ask them to be even more public in their single-payer advocacy. See the Congressional website for a list of current co-sponsors in the House and Senate.
- Seek out allied organizations, both locally and nationally, to expand the reach of your activism. Review these lists of hundreds of organizations that have endorsed Medicare for All in the House and Senate.
- Write an op-ed or letter to the editor supporting the Medicare for All Act.
Introductory town hall
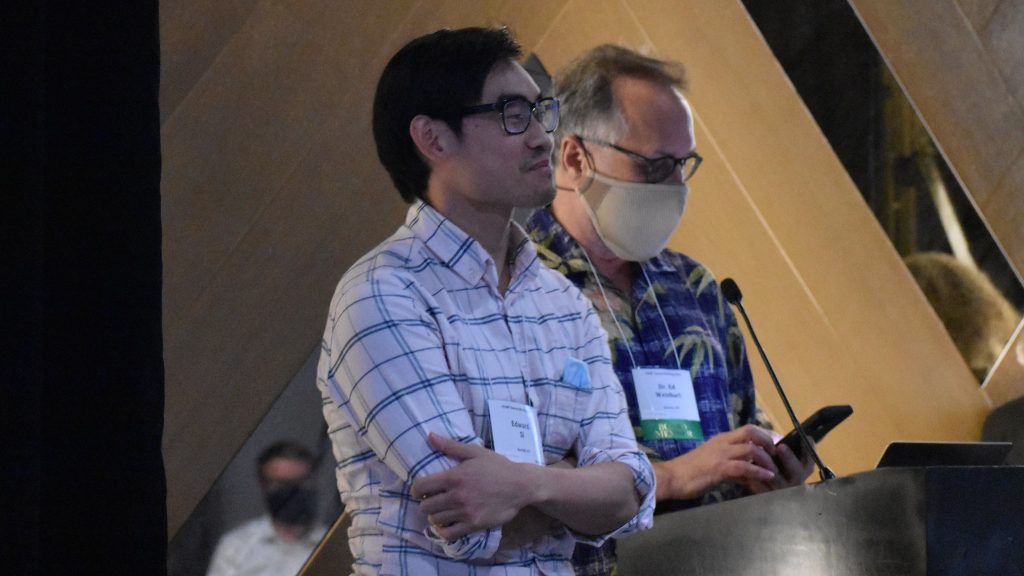
PNHP national board member Dr. Sanjeev Sriram and PNHP past president Dr. Adam Gaffney participated in a Medicare for All Town Hall with fellow health professionals and single-payer champions on May 16, 2023.
Introductory press conference
Social media graphics















 Previous Experience: At the Jane Addams Senior Caucus, I built a powerful base of leaders who were bonded not by candidates or party, but by a vision for a better future.
Previous Experience: At the Jane Addams Senior Caucus, I built a powerful base of leaders who were bonded not by candidates or party, but by a vision for a better future. Previous Experience: I previously worked in nuclear and cyber policy research at the Carnegie Endowment for International Peace in Washington, D.C.
Previous Experience: I previously worked in nuclear and cyber policy research at the Carnegie Endowment for International Peace in Washington, D.C.