PNHP’s 2024 Annual Meeting in Chicago drew physicians, students, and health justice activists from across the country for a weekend of organizing, strategizing, and setting our agenda for the year ahead.
Please see below to access a selection of archival recordings, slideshows, and handouts from the meeting. To view photos from the meeting, visit our Flickr page.
During the conference, we encouraged attendees to post to social media using the hashtag #PNHP2024. Click HERE to read member tweets, and be sure to follow PNHP on Instagram, Twitter and Facebook for the latest on the Medicare for All movement.
Looking for materials from the Students for a National Health Program (SNaHP) Summit? Click HERE to access slideshows, photos, handouts, and more!
PNHP’s “Triple Aim” to advance our movement
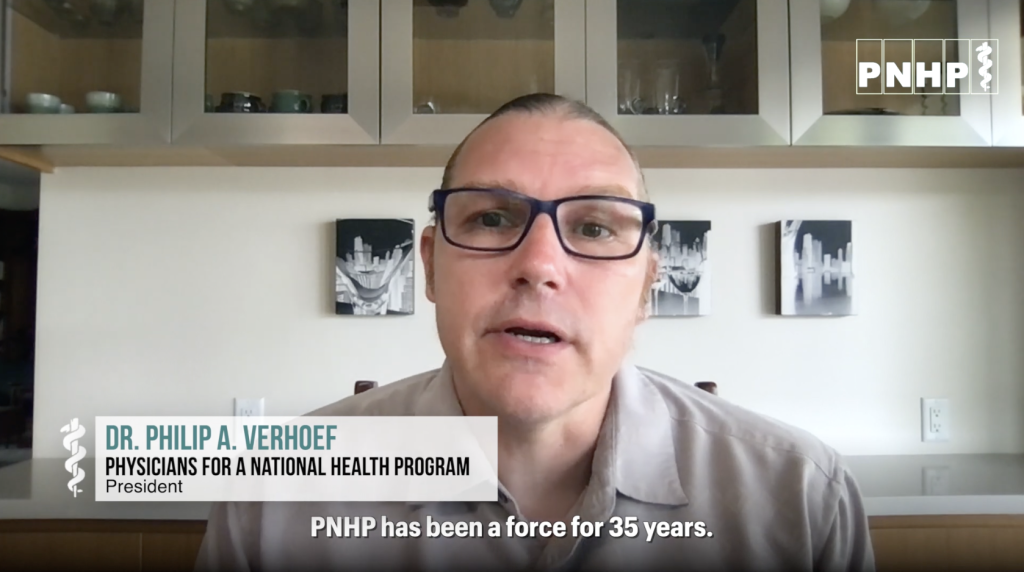
PNHP president Phil Verhoef, MD, PhD kicked off our meeting by unveiling our “Triple Aim” of ending profiteering, improving traditional Medicare, and winning single payer (slideshow HERE).
Health Policy Update
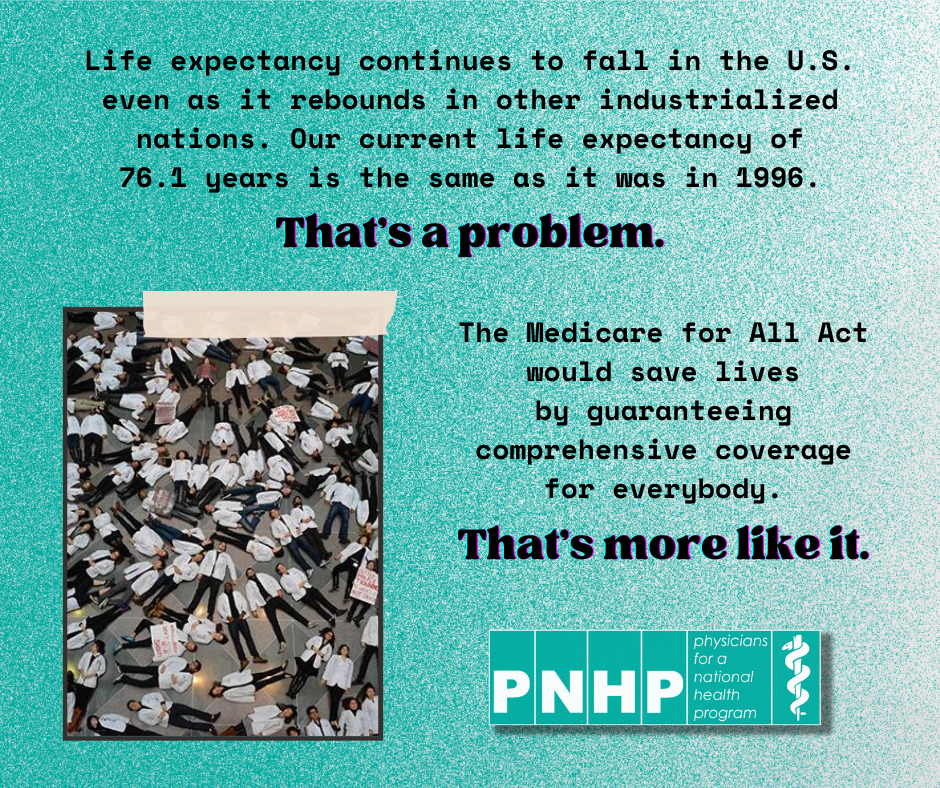
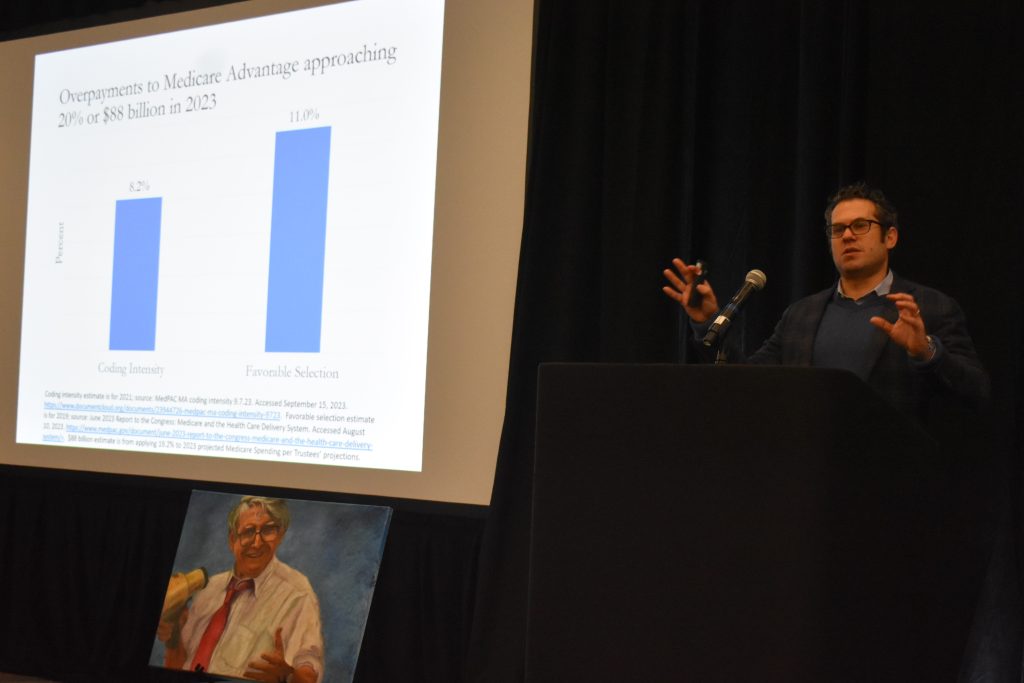
PNHP past president Adam Gaffney, MD, MPH presented the latest data on the U.S. health crisis—from declining population health, to rampant profiteering, to onerous restrictions. Download Dr. Gaffney’s original slideshow HERE or an alternate visual presentation by Dr. Ed Weisbart HERE.
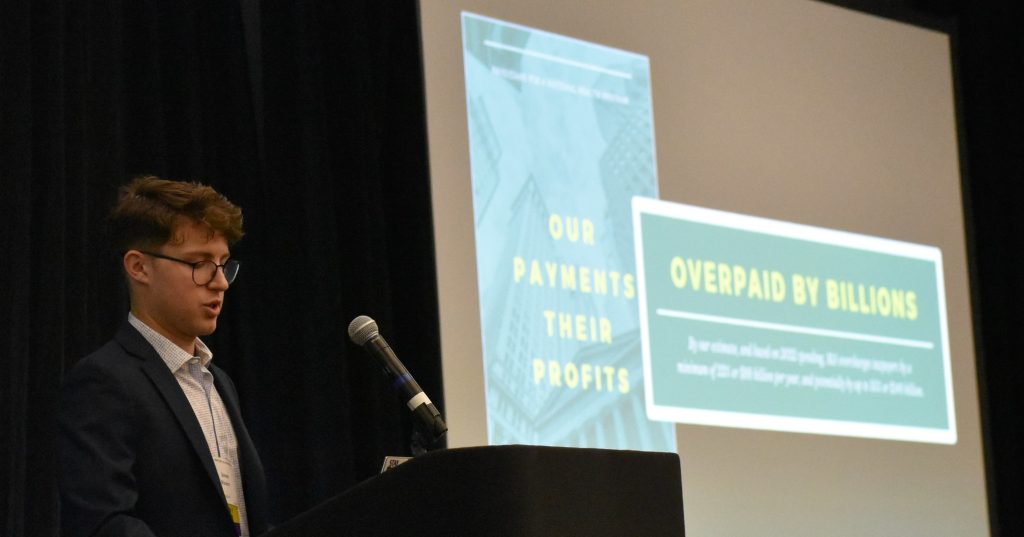
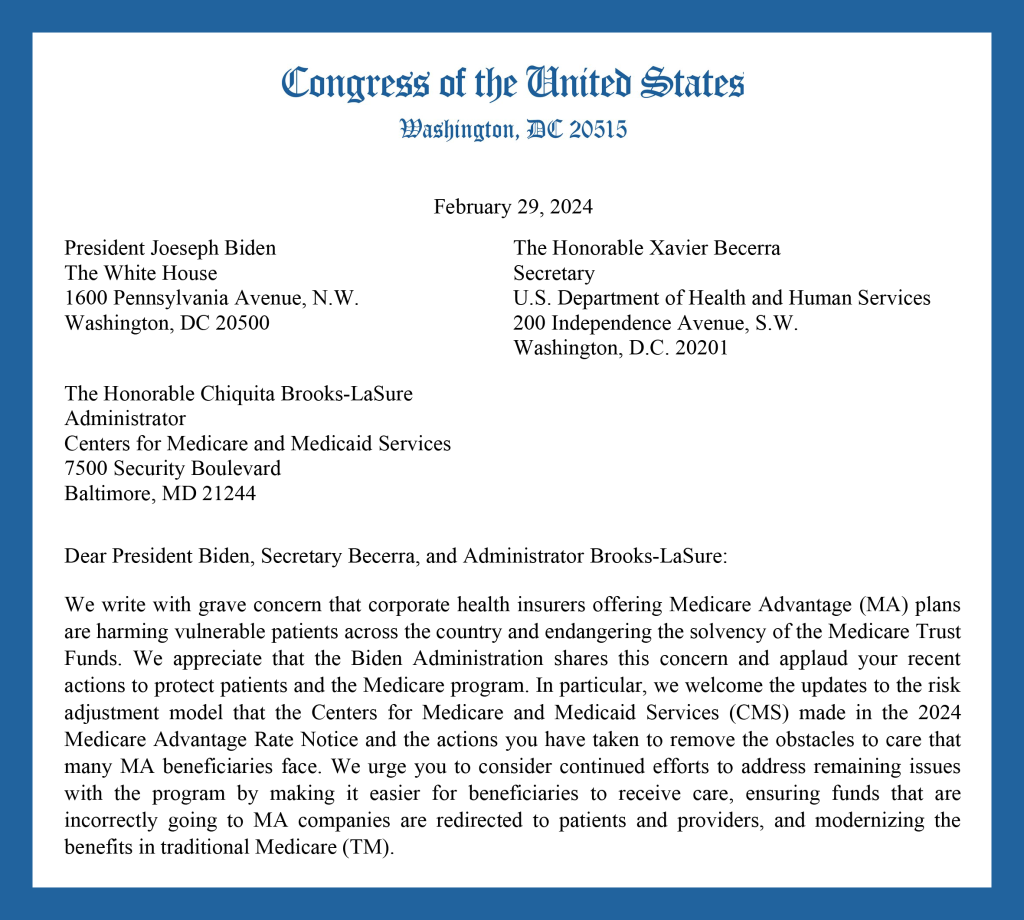
Bring Power to Truth: Fighting Medicare Advantage
SNaHP executive board members Shruthi Bhuma, M4 and Swathi Bhuma, M4 presented the main components of our campaign to stop Medicare profiteering: legislative, narrative, and organizing (slideshow HERE).
Welcome from Rep. Jan Schakowsky
Medicare for All cosponsor Rep. Jan Schakowsky (IL-9) welcomed PNHP members from across the country to Chicago, and urged us to keep pushing in the fight for single-payer reform.
Panel discussion: Reacting to the election
Featuring (R to L) Abdul El-Sayed, MD, DPhil; Alex Lawson, MPP; Wendell Potter; and A. Taylor Walker, MD, MPH. Moderated by Sanjeev Sriram, MD, MPH; and Emily Huff, M3
Workshops I: Campaigns for 2025
- Growing Power within Medical Societies, presented by Eve Shaprio, MD, MPH; Shannon Rotolo, PharmD; Stephen Kemble, MD; and Donald Bourne, M3 (worksheet HERE).
- Moral Injury: Let’s Talk About It, presented by Diljeet Singh, MD, DrPH; Carol Paris, MD; and Anand Habib, MD, MPhil (video recording HERE; slideshow HERE; worksheet HERE; moral injury survey HERE).
- A Toolbox for Building Local Power, presented by Toby Terwilliger, MD; Robel Worku; and Brooke Adams, M1 (worksheets HERE and HERE).
- Making Legislative Action Real, presented by Ed Weisbart, MD; Stephan Ramdohr; and Dan Doyle, MD (slideshow HERE; worksheet HERE).
Workshops II: Building Your Practical Skills
- Recruiting and 1:1: How to Utilize your Network, presented by Andy Hyatt, MD; Jessica Schorr Saxe, MD; and Alankrita Olson, MD (worksheet HERE).
- Tension is Part of Building Powerful Relationships of Accountability with our Legislators, presented by Hannah Willage; Belinda McIntosh, MD; and Lori Clark (slideshow HERE; worksheet HERE).
- Building Powerful Coalitions, presented by Betty Kolod, MD; Brian Yablon, MD; and Alex Newell-Taylor
- Communicating Clearly and Effectively, presented by Chiamaka Okonkwo, M4; Carol Paris, MD; Dixon Galvez-Searle; and Anika Thota (slideshow HERE; worksheet HERE; Dr. Paris’ letter to the editor HERE; moral injury survey HERE).
- Running Inclusive and Effective Meetings, presented by Zach Gallin, M4; Jenn Sugijanto, M4; and Morgan Moore (worksheets HERE and HERE).
Telling your personal health care story
Carol Paris, MD; Douglas Robinson, MD; Emily Thompson, MD; and Phil Lichtenstein, MD talk about their experiences in the exam room during our “Communicating Clearly and Effectively” workshop.
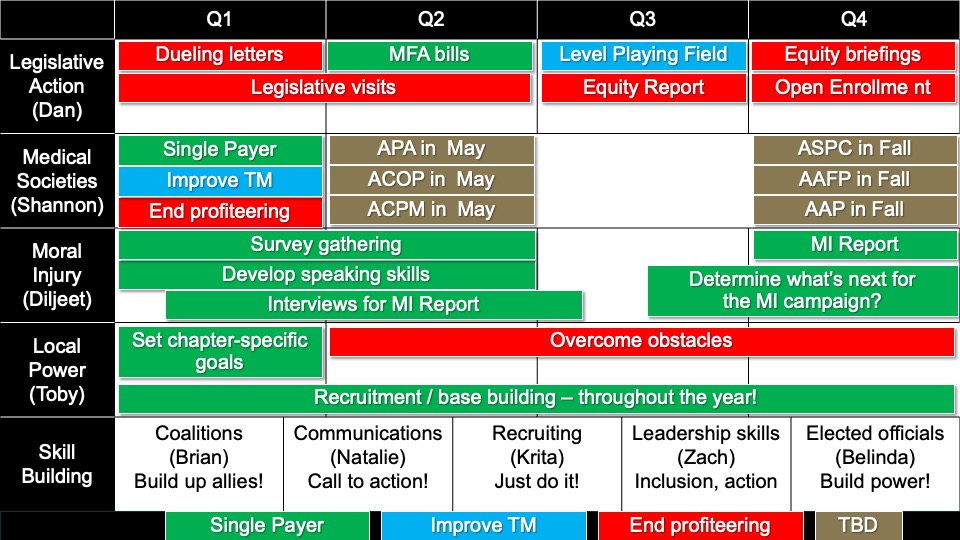
PNHP timeline for 2025
Developed by meeting attendees reporting back from our campaign and skill-building workshops. Built by Ashley Duhon, MD and Ed Weisbart, MD (recoding HERE; slideshow HERE).
Keynote: Rep. Pramila Jayapal
Congresswoman Pramila Jayapal, lead sponsor of the Medicare for All Act in the U.S. House and chair of the Congressional Progressive Caucus, concluded our meeting with a dinner keynote address.
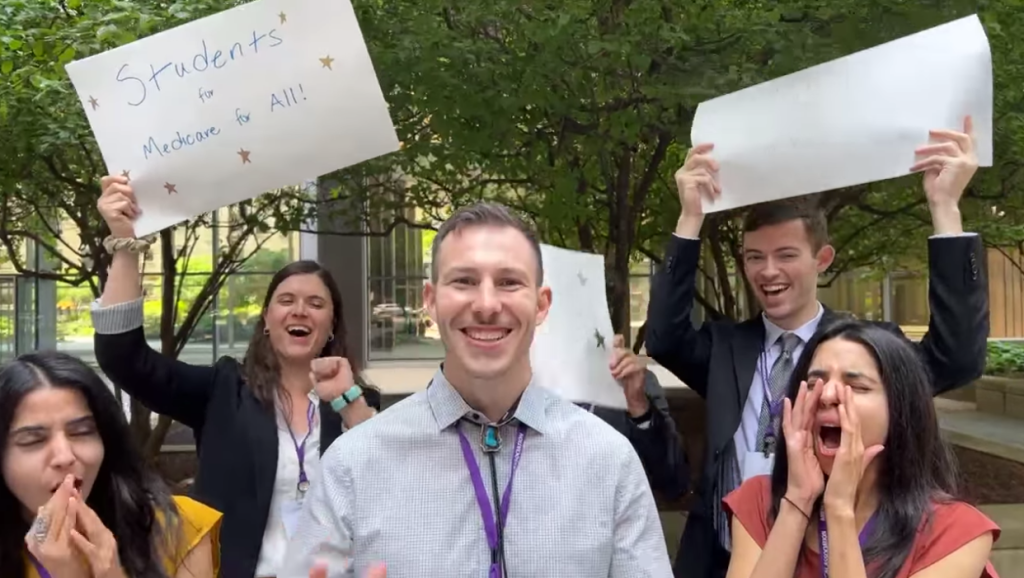
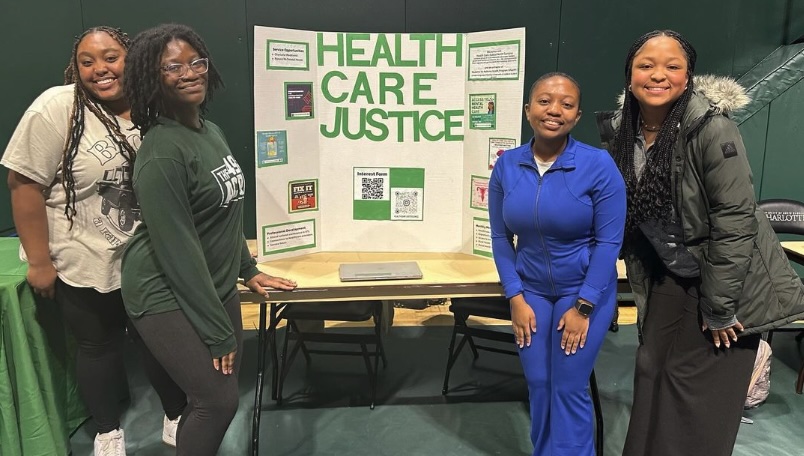
Students for a National Health Program (SNaHP) Summit
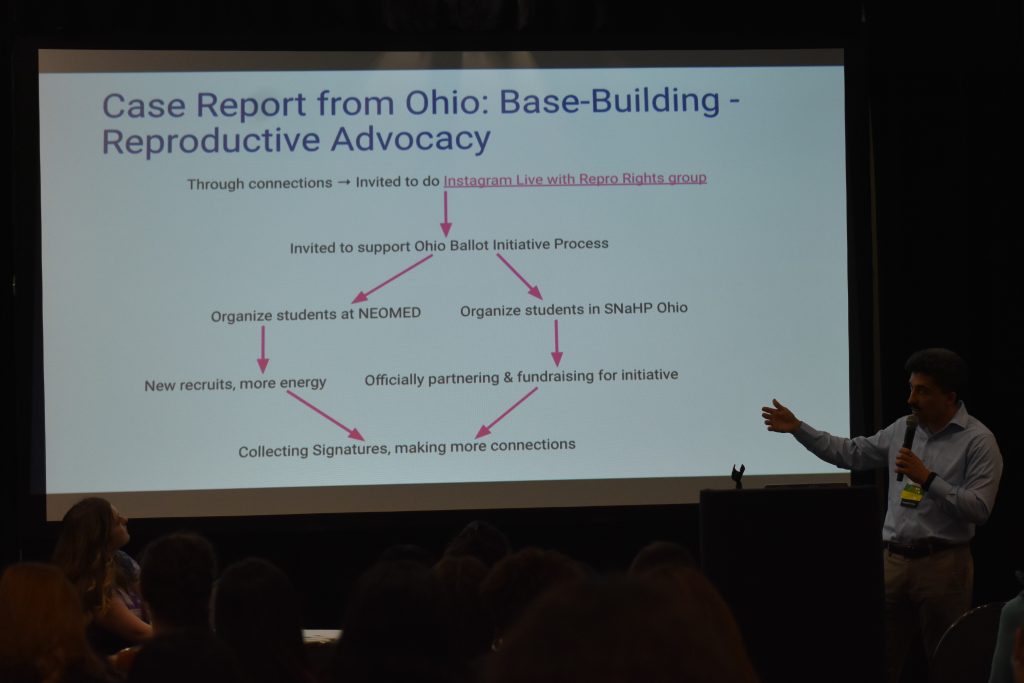
Medical and health professional students convened in Chicago for the annual SNaHP Summit on Nov. 15, 2024. During registration, students took in a wide-ranging poster presentation in the lobby.
Organizing for Human Rights
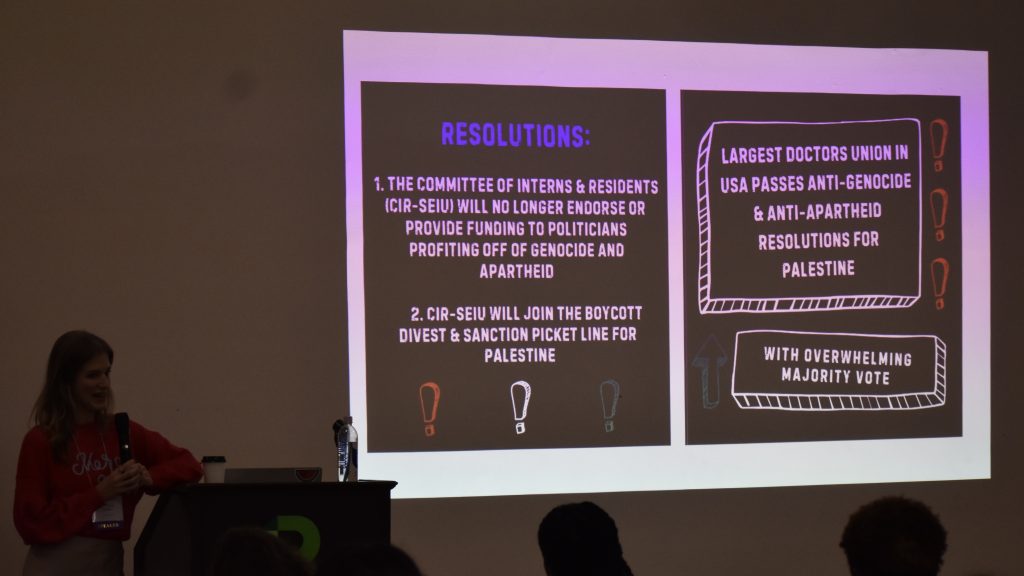
Committee of Interns and Residents president A. Taylor Walker, MD, MPH discussed her union’s organizing to pass two resolutions in support of Palestine.
Debriefing the 2024 election
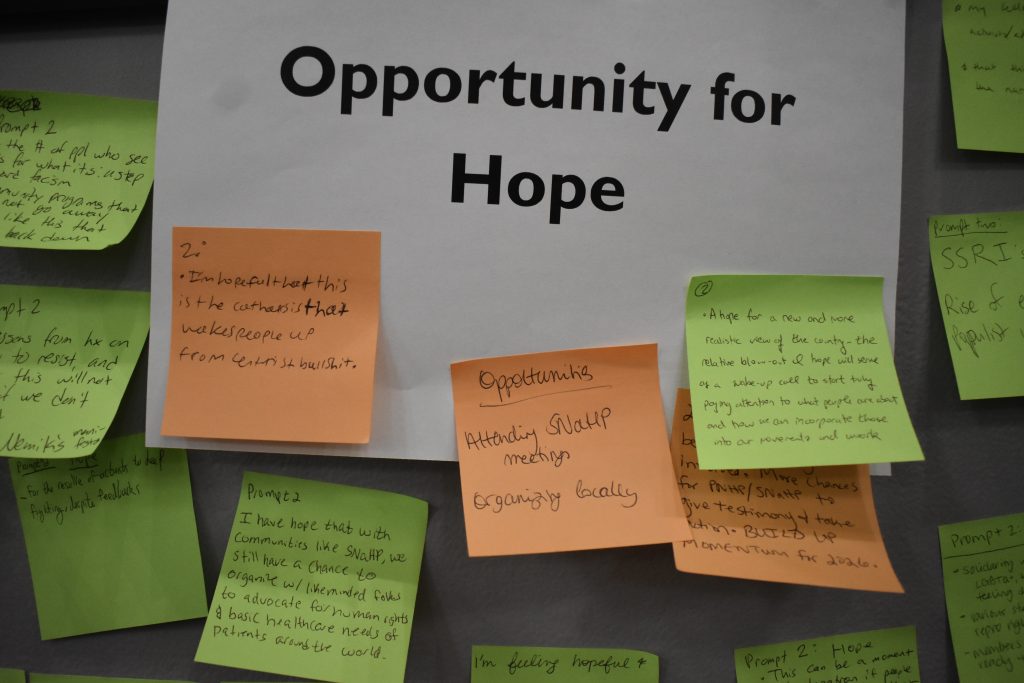
Patrick Haley and Chiamaka Okonkwo led an interactive session responding to the federal election. Students wrote down both their immediate reactions and what gave them hope in the moment.
Welcome from Rep. Delia Ramirez
Medicare for All cosponsor Rep. Delia Ramirez (IL-3) welcomed students from across the country to Chicago, the “birthplace of community organizing.”
Launching the NEW SNaHP website
SNaHP media team leaders Griffin Johnson and Natalie Koconis did their best Steve Jobs impressions while launching the revamped student.pnhp.org website.
SNaHP Strategy in 2025
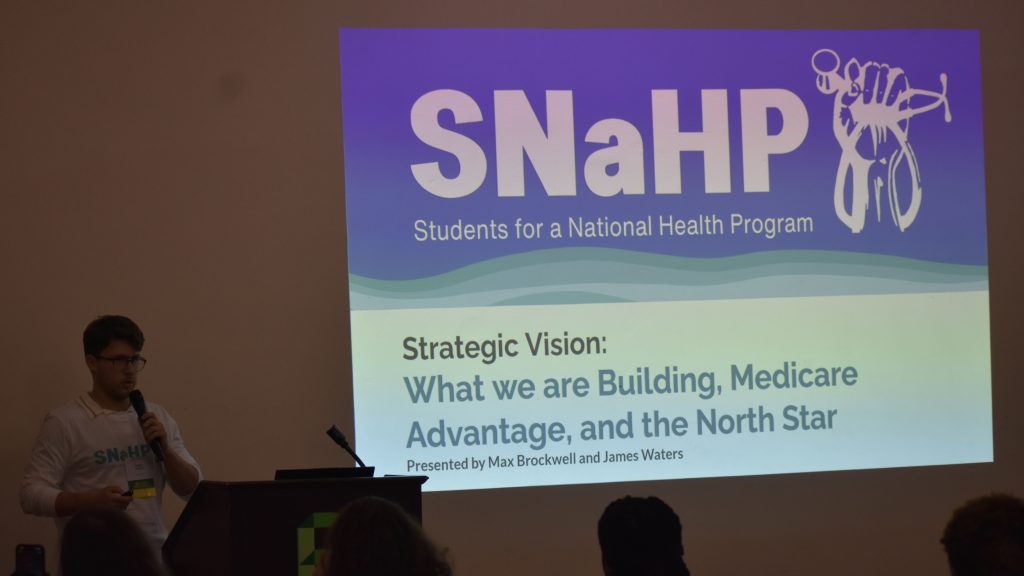
The SNaHP Summit started in earnest with presentations by Michael Massey (introduction, slideshow HERE); Shruthi and Swathi Bhuma (welcome to Chicago, slideshow HERE); Cortez Johnson (roll call); Max Brockwell and James Waters (strategic vision, slideshow HERE); and PNHP president Phil Verhoef, MD, PhD (Triple Aim, slideshow HERE).
Breakout Sessions I
- Building Statewide/Regional SNaHP Power, presented by Samuel Marquina, Gitanjali Lakshminarayanan, Carson Hartlage, Laureen Haack, and Helen Bassett (slideshow HERE)
- Start with Empathy: Talking Progress with Conservatives, presented by Cortez Johnson and John Kearney (slideshow HERE)
- Becoming Us: Building Power through Effective 1:1, presented by Andrew Meci and Annabelle Brinkerhoff (slideshow HERE; worksheet HERE)
- Writing Letters to Legislators, presented by Nina Silver, Halima Suleiman, and Priya Patel (slideshow HERE)
- The Labor Movement in Medicine: Lessons for Organizers, presented by Kevin Hu, Tom Statchen, Andy Hyatt, and A. Taylor Walker (slideshow HERE)
Breakout Sessions II
- Building A Powerful SNaHP Chapter, presented by Patrick Haley, Pritom Karmaker, and Mariam Tadross (slideshow HERE)
- The Power of Campaign Building and Plans: How We Win, presented by Max Brockwell and Chiamaka Okonkwo (slideshow HERE)
- Building knowledge about single-payer inside and outside of your med school curriculum, presented by Michael Massey and Constance Fontanet (slideshow HERE; worksheet HERE)
- Post Election Debrief: Connect, Reflect, What’s Next, presented by James Moore and Wade Catt (slideshow HERE)
- Becoming Us: Developing Powerful Testimony, presented by Donald Bourne, Carson Hartlage, Emily Huff, Allison Benjamin, Ksenia Varlyguina, and Mo Kinsinger (slideshow HERE)
Call to Action!
Shruthi and Swathi Bhuma (slideshow HERE); Allison M. Benjamin and Nina Silver; and Michael Massey led an interactive session where students made commitments to build power, take action, and work towards our North Star of Medicare for All.



 Matthew Petty
Matthew Petty Ananiya Asrat
Ananiya Asrat




 Dinner Keynote
Dinner Keynote


















 Keynote Speaker
Keynote Speaker Health Policy Update
Health Policy Update Messaging Medicare Advantage
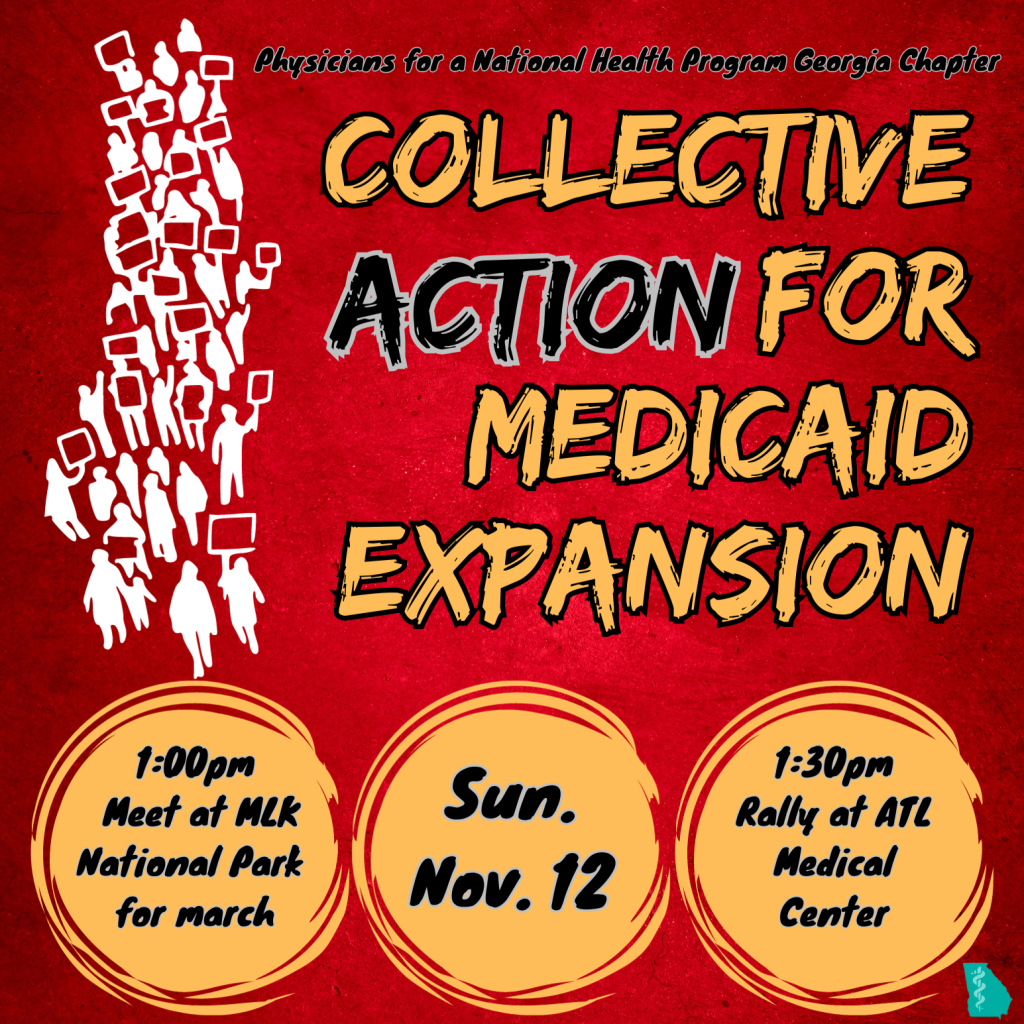
Messaging Medicare Advantage Building Progressive Power, Lessons from Georgia
Building Progressive Power, Lessons from Georgia